Table of Contents |
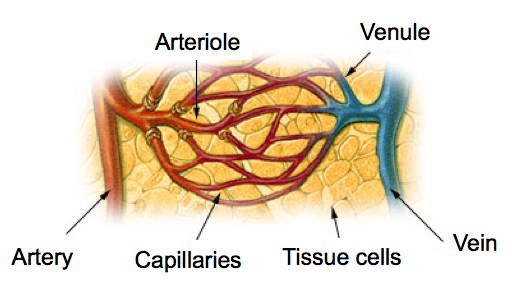
As you have learned, the different types of blood vessels work together to transport the blood that is pumped by the heart. This lesson will describe the different types of blood vessels and their functions. The diagram below shows how the types of blood vessels are connected.
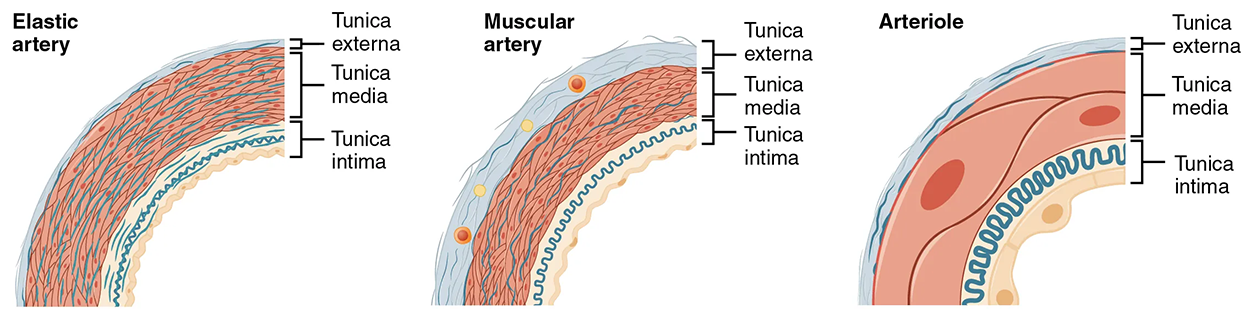
Recall that an artery is a blood vessel that conducts blood away from the heart. Each blood circuit begins with a single artery that splits to become many arteries. All arteries have relatively thick walls that can withstand the high pressure of blood ejected from the heart. However, arteries close to the heart transport the greatest amount of blood and therefore have the thickest walls to sustain the internal pressure. This type of artery is known as an elastic artery, named so because of the relatively high amount of elastic fibers found in their tunics.
These elastic fibers allow them to expand as blood passes through them and then to recoil after the surge has passed. If artery walls were rigid and unable to expand and recoil, their resistance to blood flow would greatly increase. The elastic recoil of the vascular wall helps to maintain the pressure gradient that drives the blood through the arterial system. An elastic artery is also known as a conducting artery because the large diameter of the lumen (>10 mm) enables it to accept a large volume of blood from the heart and conduct it to smaller branches.
Farther from the heart, the systemic circuit splits, which dampens the surge of blood. These arteries are smaller (ranging from 0.1 to 10 mm) and have fewer elastic fibers due to decreased internal blood pressure. They also contain an increased percentage of smooth muscle in the tunica media, which allows the blood vessel to vasoconstrict and vasodilate. The artery at this point is described as a muscular artery. Because the blood pressure has eased by the time it reaches these more distant vessels, elasticity has become less important.
An arteriole is a very small artery that leads to a capillary. Arterioles have the same three tunics as the larger vessels, but the thickness of each is greatly diminished. The critical endothelial lining of the tunica interna is intact. The tunica media is restricted to one or two smooth muscle cell layers in thickness. The tunica externa remains but is very thin (see the figure above).
With a lumen averaging 30 micrometers or less in diameter, arterioles are critical in slowing down—or resisting—blood flow and thus causing a substantial drop in blood pressure. Because of this, you may see them referred to as resistance vessels. The muscle fibers in arterioles are normally slightly contracted, causing arterioles to maintain a consistent muscle tone—in this case, referred to as vascular tone—in a similar manner to the muscular tone of skeletal muscle. In reality, all blood vessels exhibit vascular tone due to the partial contraction of smooth muscle. The importance of the arterioles is that they will be the primary site of both resistance and regulation of blood pressure.
The precise diameter of the lumen of an arteriole at any given moment is determined by neural and chemical controls, and vasoconstriction and vasodilation in the arterioles are the primary mechanisms for the distribution of blood flow.
A capillary is a microscopic channel that supplies blood to the tissues. Exchange of gases and other substances occurs between the blood in capillaries and the surrounding cells and their tissue fluid (interstitial fluid). As you may recall from red blood cells, some capillaries are barely wide enough for a red blood cell to squeeze through, ranging from 5–10 micrometers.
For capillaries to function, their walls must be leaky, allowing substances to pass through. The wall of a capillary consists of the endothelial layer (tunica interna) surrounded by a basement membrane with occasional smooth muscle fibers. There are three major types of capillaries, which differ according to their degree of “leakiness”: continuous, fenestrated, and sinusoid capillaries.
The most common type of capillary, the continuous capillary is characterized by a complete endothelial lining with tight junctions between endothelial cells. Although a tight junction is usually impermeable and only allows for the passage of water and ions, they are often incomplete in capillaries, leaving intercellular clefts that allow for the exchange of water and other very small molecules between the blood plasma and the interstitial fluid. Substances that can pass between cells include metabolic products, such as glucose, water, and small hydrophobic molecules like gases and hormones, as well as various leukocytes. Continuous capillaries in the brain are part of the blood–brain barrier. Here, there are tight junctions and no intercellular clefts, plus a thick basement membrane and astrocyte extensions called end feet; these structures combine to prevent the movement of nearly all substances.
A fenestrated capillary is one that has pores (or fenestrations) in addition to tight junctions in the endothelial lining. These make the capillary permeable to larger molecules. The number of fenestrations and their degree of permeability vary, however, according to their location. Fenestrated capillaries are common in the small intestine, which is the primary site of nutrient absorption, as well as in the kidneys, which filter the blood. They are also found in the choroid plexus of the brain and many endocrine structures, including the hypothalamus, pituitary, pineal, and thyroid glands.
A sinusoid capillary (or sinusoid) is the least common type of capillary. Sinusoid capillaries are flattened, and they have extensive intercellular gaps and incomplete basement membranes, in addition to intercellular clefts and fenestrations. This gives them an appearance not unlike Swiss cheese. These very large openings allow for the passage of the largest molecules, including plasma proteins and even cells. Blood flow through sinusoid capillaries is very slow, allowing more time for the exchange of gases, nutrients, and wastes. Sinusoids are found in the liver and spleen, bone marrow, lymph nodes (where they carry lymph, not blood), and many endocrine glands, including the pituitary and adrenal glands. Without these specialized capillaries, these organs would not be able to provide their myriad functions.
EXAMPLE
When bone marrow forms new blood cells, the cells must enter the blood supply and can only do so through the large openings of a sinusoid capillary; they cannot pass through the small openings of continuous or fenestrated capillaries.The liver also requires extensive specialized sinusoid capillaries to process the materials brought to it by the hepatic portal vein from both the digestive tract and spleen and to release plasma proteins into circulation.
Each terminal arteriole branches to supply blood to a capillary bed that may consist of 10–100 capillaries. To regulate blood movement through these complex series of vessels, there are precapillary sphincters, circular smooth muscle cells that surround the capillary at its origin. Their function is critical: If all of the capillary beds in the body were to open simultaneously, they would collectively hold every drop of blood in the body and there would be none in the arteries, arterioles, venules, veins, or the heart itself.
Normally, the precapillary sphincters are closed. When the surrounding tissues need oxygen and have excess waste products, the precapillary sphincters open, allowing blood to flow through and exchange to occur before closing once more. If all of the precapillary sphincters in a capillary bed are closed, blood will flow directly into a thoroughfare channel and then into the venous circulation, bypassing the capillary bed entirely. This creates what is known as a vascular shunt. In addition, an arteriovenous anastomosis may bypass the capillary bed and lead directly to the venous system.
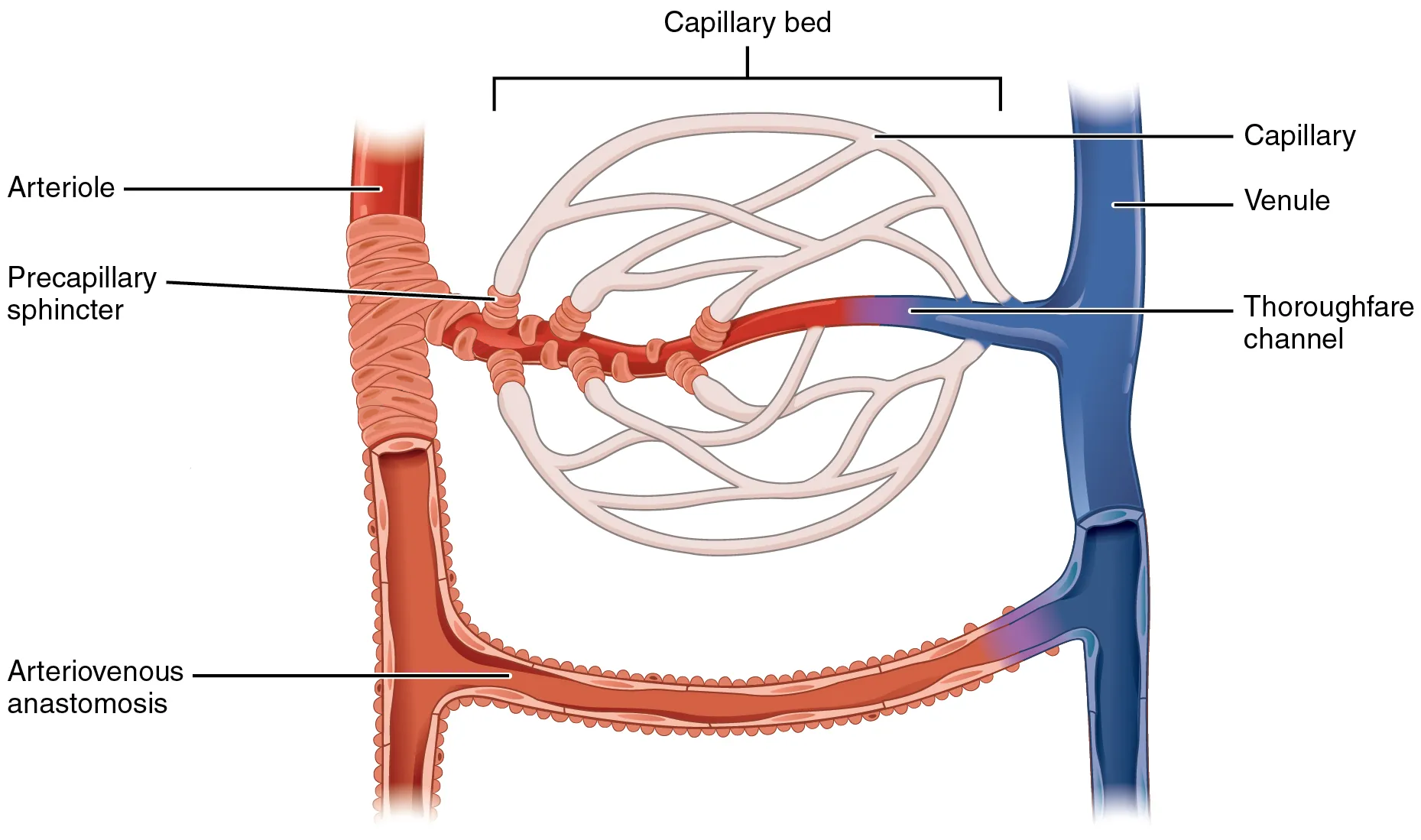
Although you might expect blood flow through a capillary bed to be smooth, in reality, it moves with an irregular, pulsating flow. This pattern is called vasomotion and is regulated by chemical signals that are triggered in response to changes in internal conditions, such as oxygen, carbon dioxide, hydrogen ion, and lactic acid levels.
EXAMPLE
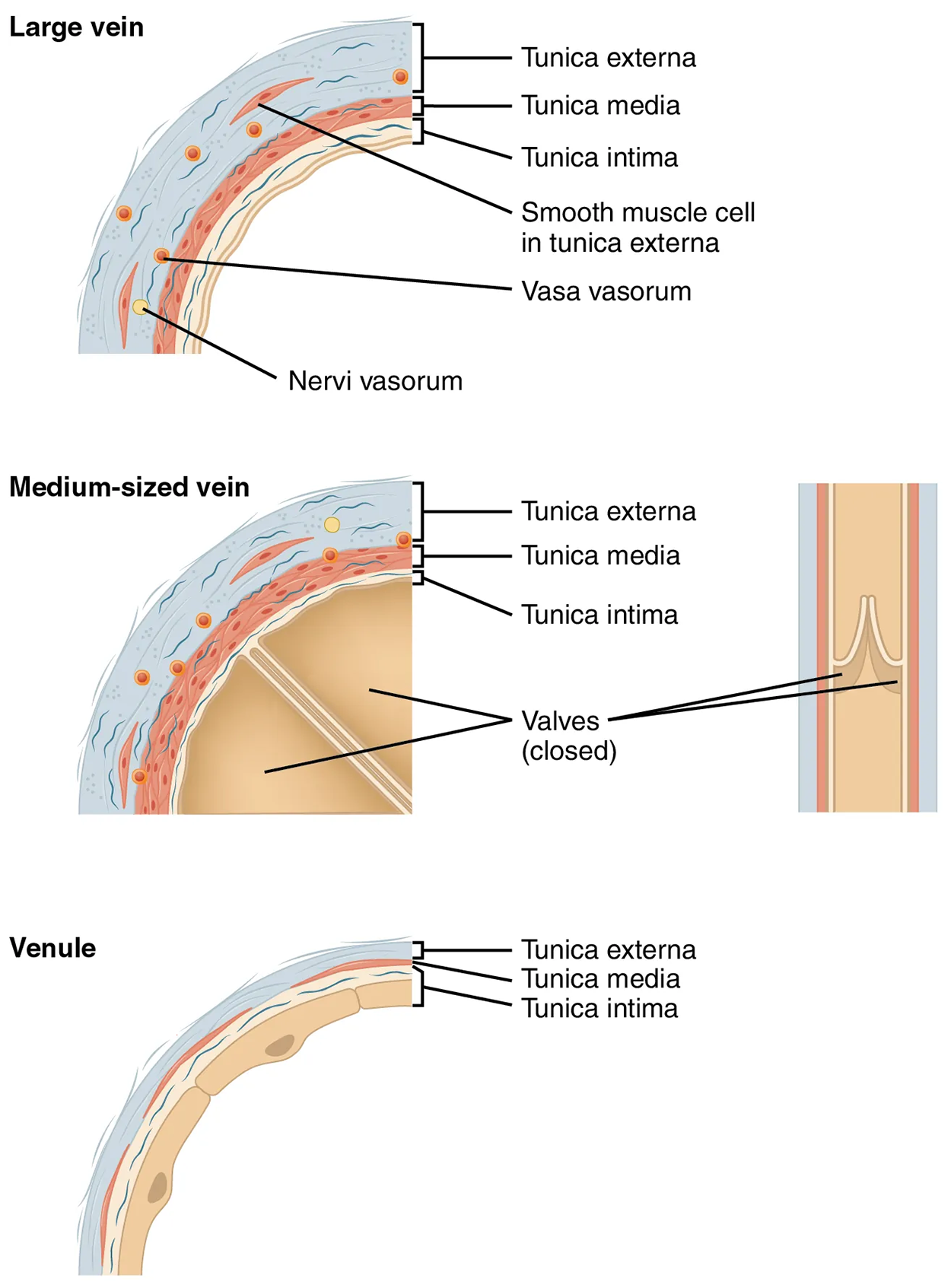
During strenuous exercise, when oxygen levels decrease and carbon dioxide, hydrogen ion, and lactic acid levels all increase, the capillary beds in skeletal muscle are open, as they would be in the digestive system when nutrients are present in the digestive tract. During sleep or rest periods, vessels in both areas are largely closed; they open only occasionally to allow oxygen and nutrient supplies to travel to the tissues to maintain basic life processes.A venule is an extremely small vein, generally 8–100 micrometers in diameter. Venules join together multiple capillaries exiting from a capillary bed. Multiple venules join to form veins. The walls of venules consist of endothelium, a thin middle layer with a few muscle cells and elastic fibers, plus an outer layer of connective tissue fibers that constitute a very thin tunica externa. Venules as well as capillaries are the primary sites of emigration or diapedesis, in which the white blood cells adhere to the endothelial lining of the vessels and then squeeze through adjacent cells to enter the tissue fluid.
A vein is a blood vessel that conducts blood toward the heart. Compared with arteries, veins are thin-walled vessels with large and irregular lumens. Because they are low-pressure vessels, larger veins are commonly equipped with valves (shown below) that promote the unidirectional flow of blood toward the heart and prevent backflow toward the capillaries caused by the inherent low blood pressure in veins as well as the pull of gravity. The table below compares the features of arteries and veins.
| Comparison of Arteries and Veins | ||
|---|---|---|
| Arteries | Veins | |
| Direction of blood flow | Conducts blood away from the heart | Conducts blood toward the heart |
| General appearance | Rounded | Irregular, often collapsed |
| Pressure | High | Low |
| Wall thickness | Thick | Thin |
| Relative oxygen concentration |
Higher in systemic arteries Lower in pulmonary arteries |
Lower in systemic veins Higher in pulmonary veins |
| Valves | Not present | Present most commonly in limbs and in veins inferior to the heart |
In addition to their primary function of returning blood to the heart, veins may be considered blood reservoirs because systemic veins contain approximately 64% of the blood volume at any given time. Their ability to hold this much blood is due to their high capacitance, that is, their capacity to distend (expand) readily to store a high volume of blood, even at a low pressure. The large lumens and relatively thin walls of veins make them far more distensible than arteries; thus, they are said to be capacitance vessels.
When blood flow needs to be redistributed to other portions of the body, the vasomotor center located in the medulla oblongata (the inferior portion of the brain stem) sends sympathetic stimulation to the smooth muscles in the walls of the veins, causing constriction—or in this case, venoconstriction. Less dramatic than the vasoconstriction seen in smaller arteries and arterioles, venoconstriction may be likened to a “stiffening” of the vessel wall. This increases pressure on the blood within the veins, speeding its return to the heart.
Approximately 21% of the venous blood is located in venous networks within the liver, bone marrow, and integument. This volume of blood is referred to as venous reserve. Through venoconstriction, this “reserve” volume of blood can get back to the heart more quickly for redistribution to other parts of the circulation.
IN CONTEXT
Career Connection
Vascular Surgeons and Technicians
Vascular surgery is a specialty in which the physician deals primarily with diseases of the vascular portion of the cardiovascular system. This includes repair and replacement of diseased or damaged vessels, removal of plaque from vessels, minimally invasive procedures including the insertion of venous catheters, and traditional surgery. Following completion of medical school, the physician generally completes a 5-year surgical residency followed by an additional 1 to 2 years of vascular specialty training. In the United States, most vascular surgeons are members of the Society of Vascular Surgery.
Vascular technicians are specialists in imaging technologies that provide information on the health of the vascular system. They may also assist physicians in treating disorders involving the arteries and veins. This profession often overlaps with cardiovascular technology, which would also include treatments involving the heart. Although recognized by the American Medical Association, there are currently no licensing requirements for vascular technicians, and licensing is voluntary. Vascular technicians typically have an associate’s degree or certificate, involving 18 months to 2 years of training.
SOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM (1) OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION. (2) OPENSTAX “MICROBIOLOGY”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/MICROBIOLOGY/PAGES/1-INTRODUCTION. LICENSING (1 & 2): CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.