Table of Contents |
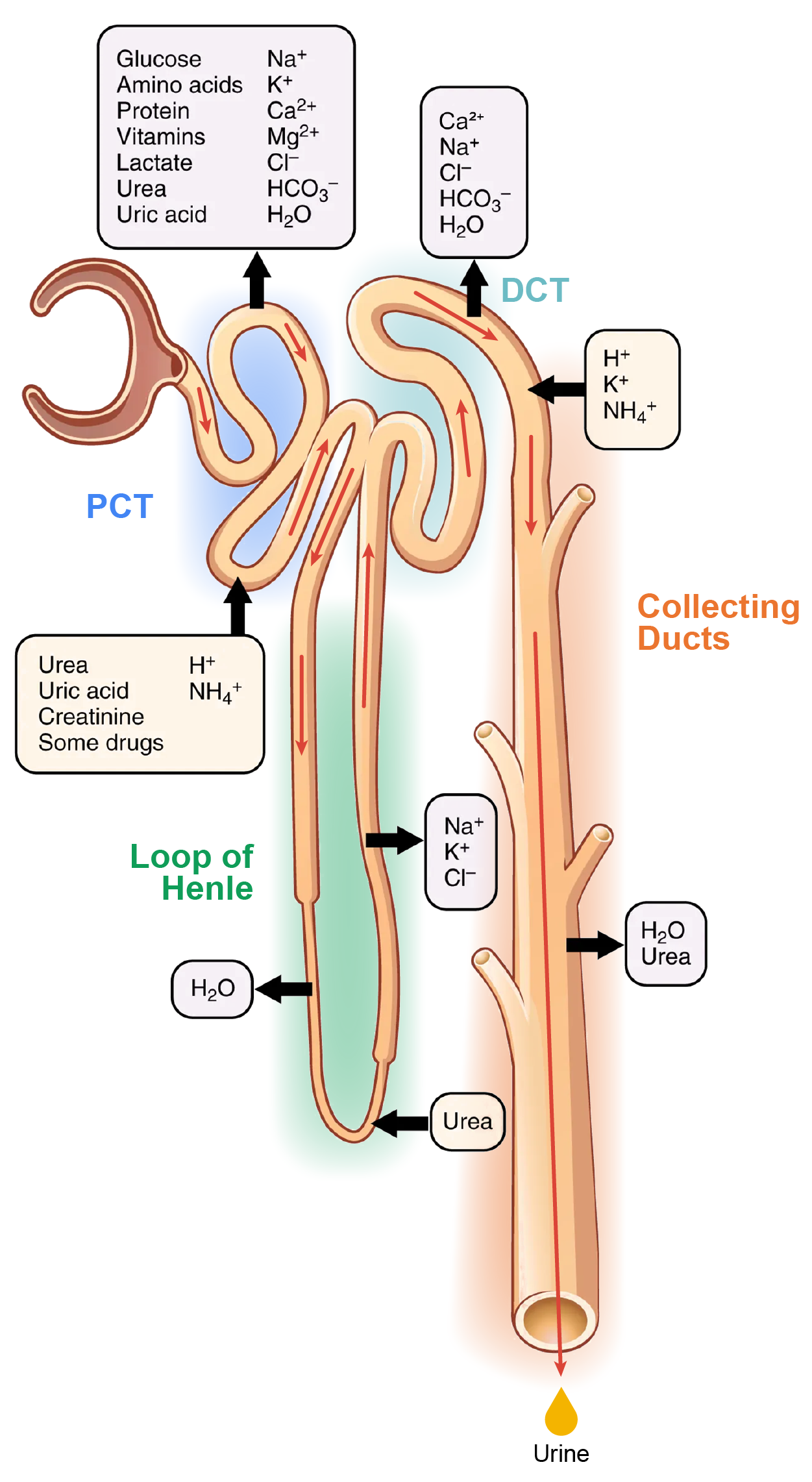
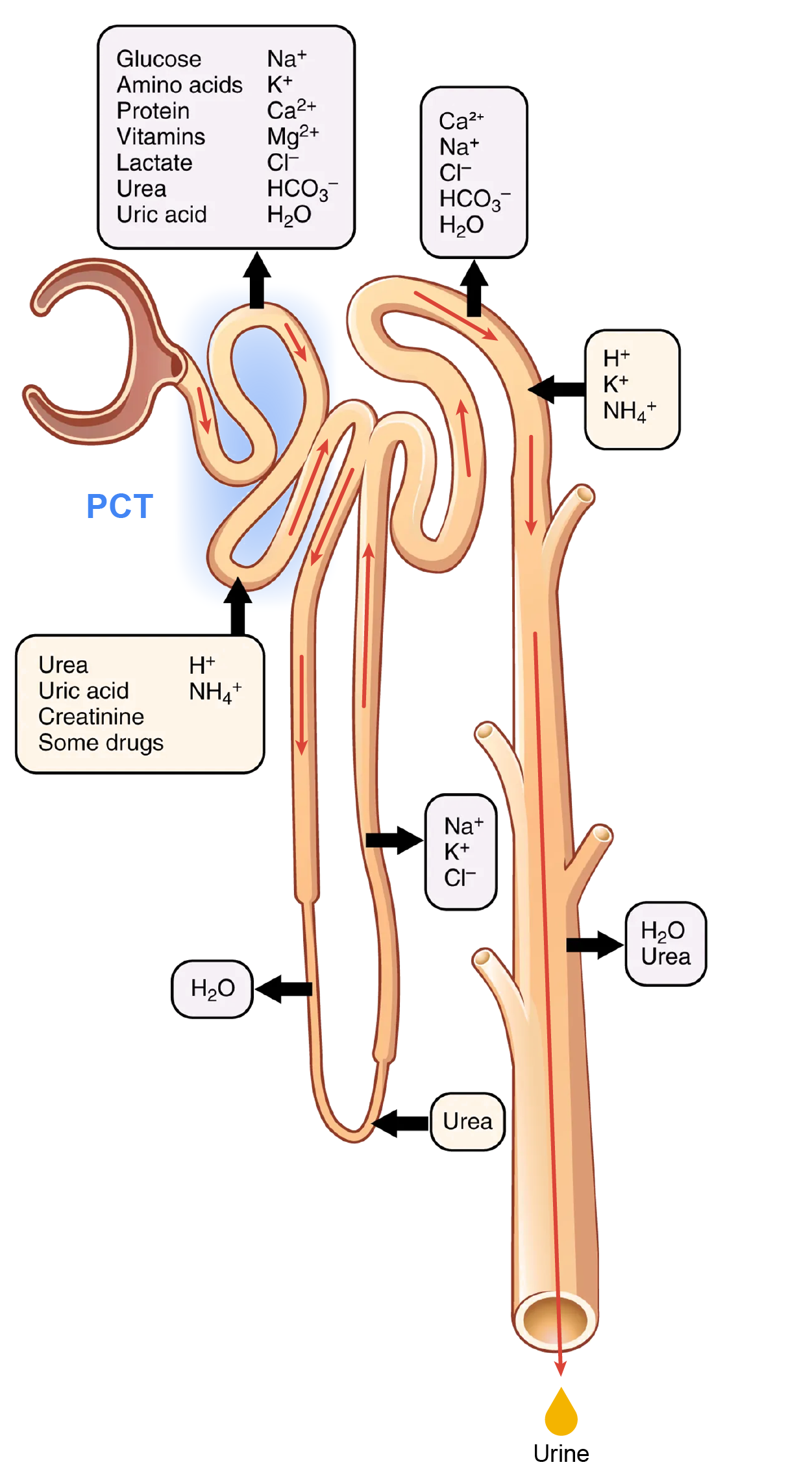
With up to 180 L per day passing through the nephrons of the kidney, it is quite obvious that most of that fluid and its contents must be reabsorbed. That recovery occurs in the proximal convoluted tubule (PCT) and loop of Henle, and fluid balance and secretion occur in the distal convoluted tubule (DCT) and collecting ducts (see the areas in the image below). Various portions of the nephron differ in their capacity to reabsorb water and specific solutes.
While much of the reabsorption and secretion occur passively based on concentration gradients, the amount of water that is reabsorbed or lost is tightly regulated. This control is exerted directly by antidiuretic hormone (ADH) and aldosterone, and indirectly by renin.
Recall that in a previous lesson, you learned that ADH is a hormone secreted by the hypothalamus that signals water reabsorption by the kidneys. Most water is recovered in the PCT, loop of Henle, and DCT. About 10% (about 18 L) reaches the collecting ducts. The collecting ducts, under the influence of ADH, can recover almost all of the water passing through them, in cases of dehydration, or almost none of the water, in cases of overhydration.
Mechanisms by which substances move across membranes for reabsorption or secretion include active transport, diffusion, facilitated diffusion, secondary active transport, and osmosis.
Active transport utilizes energy, usually the energy found in a phosphate bond of ATP, to move a substance across a membrane from a low to a high concentration. It is very specific and must have an appropriately shaped receptor for the substance to be transported. The transport of Na⁺ out of a cell and K⁺ into a cell by the Na⁺/K⁺ pump is an example of active transport. Both ions are moved in opposite directions from a lower to a higher concentration.
Simple diffusion moves a substance from a higher to a lower concentration down its concentration gradient. It requires no energy and only needs to be soluble.
Facilitated diffusion is similar to diffusion in that it moves a substance down its concentration gradient. The difference is that it requires specific membrane receptors or channel proteins for movement. The movement of glucose and, in certain situations, Na⁺ ions is an example of facilitated diffusion. In some cases of mediated transport, two different substances share the same channel protein port; these mechanisms are described by the terms “symport” and “antiport.”
Symport mechanisms move two or more substances in the same direction at the same time, whereas antiport mechanisms move two or more substances in opposite directions across the cell membrane. Both mechanisms may utilize concentration gradients maintained by ATP pumps. As described previously, when active transport powers the transport of another substance in this way, it is called “secondary active transport.” Glucose reabsorption in the kidneys occurs by secondary active transport. Na⁺/K⁺ ATPases on the basal membrane of a tubular cell constantly pump Na⁺ out of the cell, maintaining a strong electrochemical gradient for Na⁺ to move into the cell from the tubular lumen. On the luminal (apical) surface, a Na⁺/glucose symport protein assists both Na⁺ and glucose movement into the cell. The cotransporter moves glucose into the cell against its concentration gradient as Na⁺ moves down the electrochemical gradient created by the basal membrane's Na⁺/K⁺ ATPases. The glucose molecule then diffuses across the basal membrane by facilitated diffusion into the interstitial space and from there into peritubular capillaries.
Most of the Ca²⁺, Na⁺, glucose, and amino acids must be reabsorbed by the nephron to maintain homeostatic plasma concentrations. Other substances, such as urea, K⁺, ammonia (NH₃), creatinine, and some drugs are secreted into the filtrate as waste products. Acid–base balance is maintained through actions of the lungs and kidneys: The lungs rid the body of H⁺, whereas the kidneys secrete or reabsorb H⁺ and HCO₃⁻. In the case of urea, about 50% is passively reabsorbed by the PCT. More is recovered by the collecting ducts as needed. ADH induces the insertion of urea transporters and aquaporin channel proteins.
The renal corpuscle filters the blood to create a filtrate that differs from blood mainly in the absence of cells and large proteins. From this point to the ends of the collecting ducts, the filtrate undergoes modification through secretion and reabsorption before true urine is produced.
The first point at which the forming urine is modified is in the PCT. Here, some substances are reabsorbed, whereas others are secreted. Note the use of the term “reabsorbed.” All of these substances were “absorbed” in the digestive tract—99% of the water and most of the solutes filtered by the nephron must be reabsorbed. Water and substances that are reabsorbed are returned to the circulation by the peritubular and vasa recta capillaries. The peritubular capillaries surround the PCT and DCT, and they are associated with the vasa recta capillaries, which surround the loop of Henle.
In the PCT, approximately ⅔ of the filtered Na⁺, K⁺, and H₂O are reabsorbed. All of the filtered glucose is reabsorbed. Most bicarbonate (80–90%) is reabsorbed. Phosphate (85%) is reabsorbed but inhibited by parathyroid hormone (PTH).
The loop of Henle consists of two sections: thick and thin descending and thin and thick ascending sections. The loops of cortical nephrons do not extend into the renal medulla very far, if at all. Juxtamedullary nephrons have loops that extend variable distances, some very deep into the medulla. The descending and ascending portions of the loop are highly specialized to enable the recovery of much of the Na⁺ and water that was filtered by the glomerulus.
As the forming urine moves through the loop, the osmolarity will change from isosmotic with blood (about 278–300 mOsmol/kg) to both a very hypertonic solution of about 1200 mOsmol/kg and a very hypotonic solution of about 100 mOsmol/kg. These changes are accomplished by osmosis in the descending limb and active transport in the ascending limb. Solutes and water recovered from these loops are returned to the circulation by way of the vasa recta.
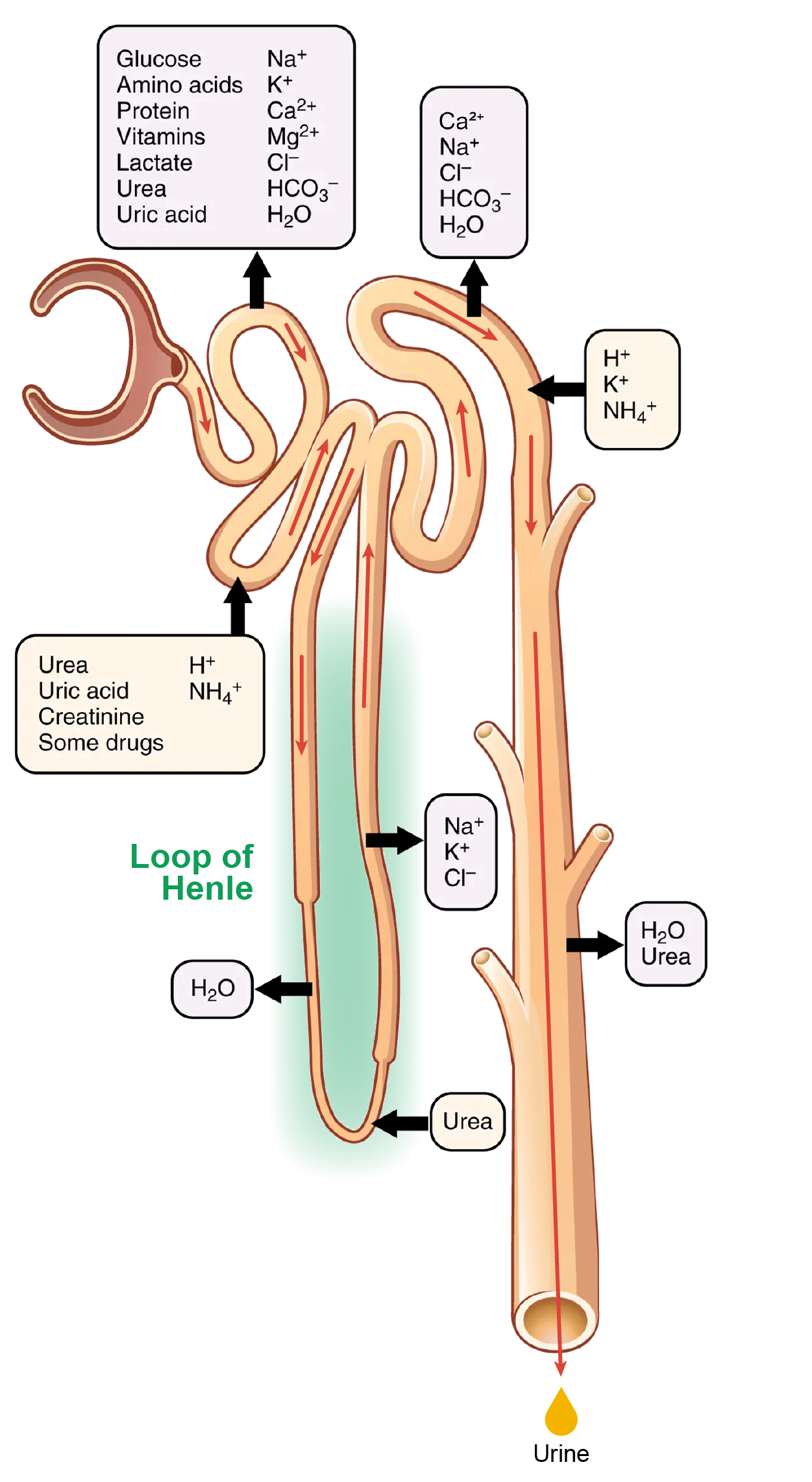
The structure of the loop of Henle and associated vasa recta create a countercurrent multiplier system. The countercurrent term comes from the fact that the descending and ascending loops are next to each other and their fluid flows in opposite directions (countercurrent). The multiplier term is because of the action of solute pumps that increase (multiply) the concentrations of urea and Na⁺ deep in the medulla.
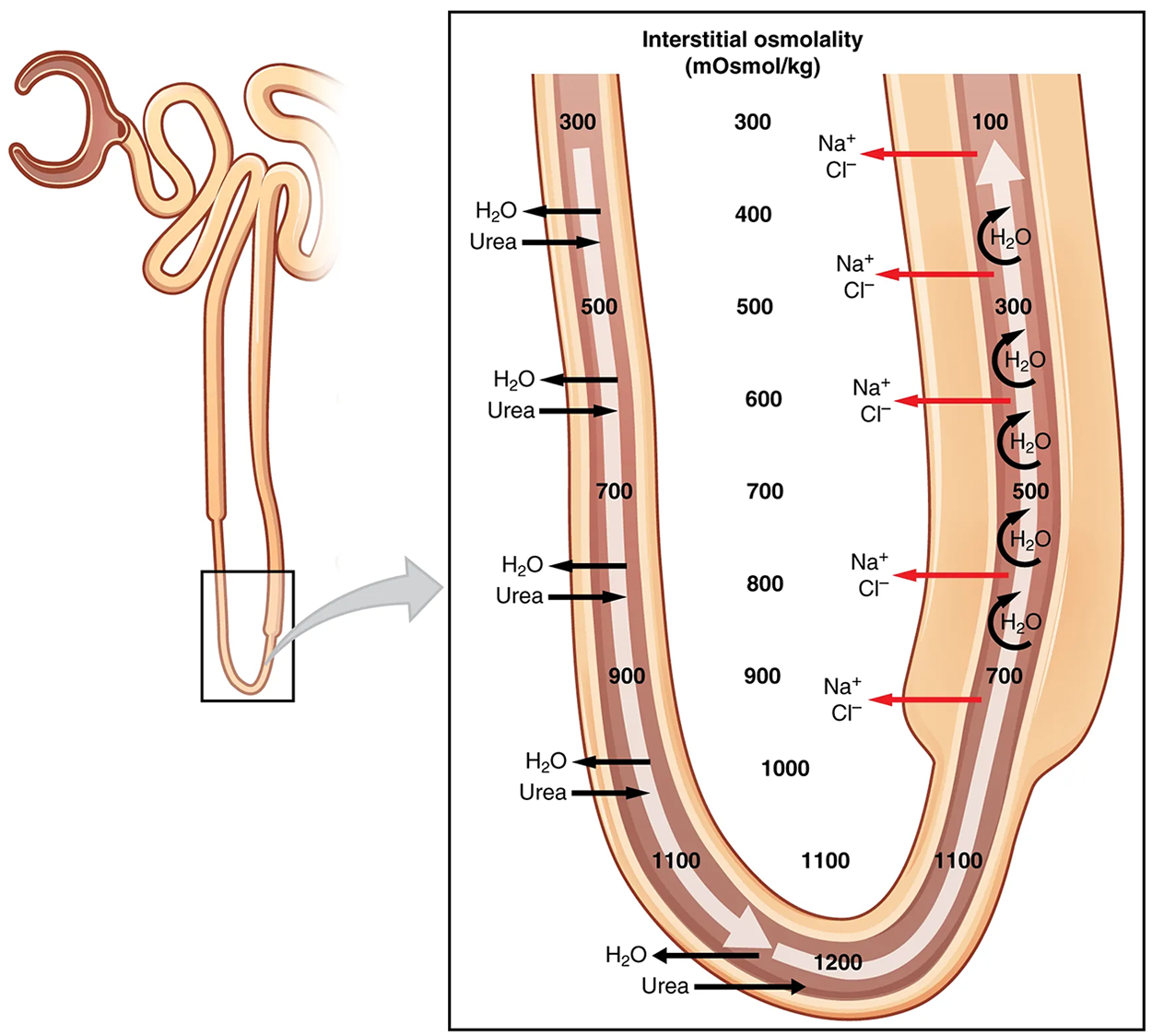
As discussed above, the ascending loop actively reabsorbs NaCl out of the forming urine into the interstitial spaces. In addition, collecting ducts have urea pumps that actively pump urea into the interstitial spaces. This results in the recovery of NaCl to the circulation via the vasa recta and creates a high osmolar environment in the depths of the medulla.
Approximately 80% of filtered water has been recovered by the time the dilute forming urine enters the DCT.
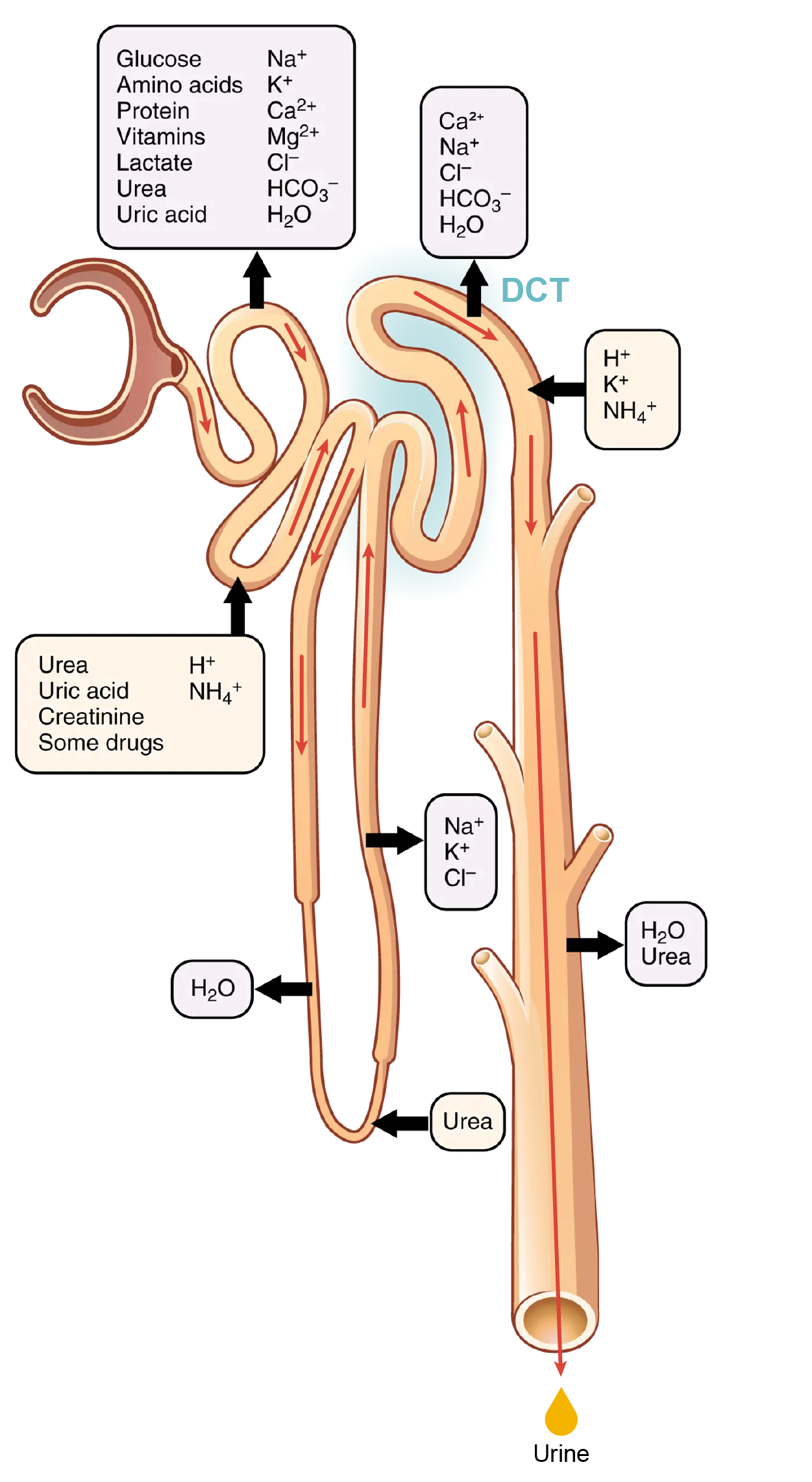
What is happening in the early DCT:
Solutes move across the membranes of the collecting ducts, which contain two distinct cell types, principal cells and intercalated cells. A principal cell possesses channels for the recovery or loss of sodium and potassium. An intercalated cell secretes or absorbs acid or bicarbonate. As in other portions of the nephron, there is an array of micromachines (pumps and channels) on display in the membranes of these cells.
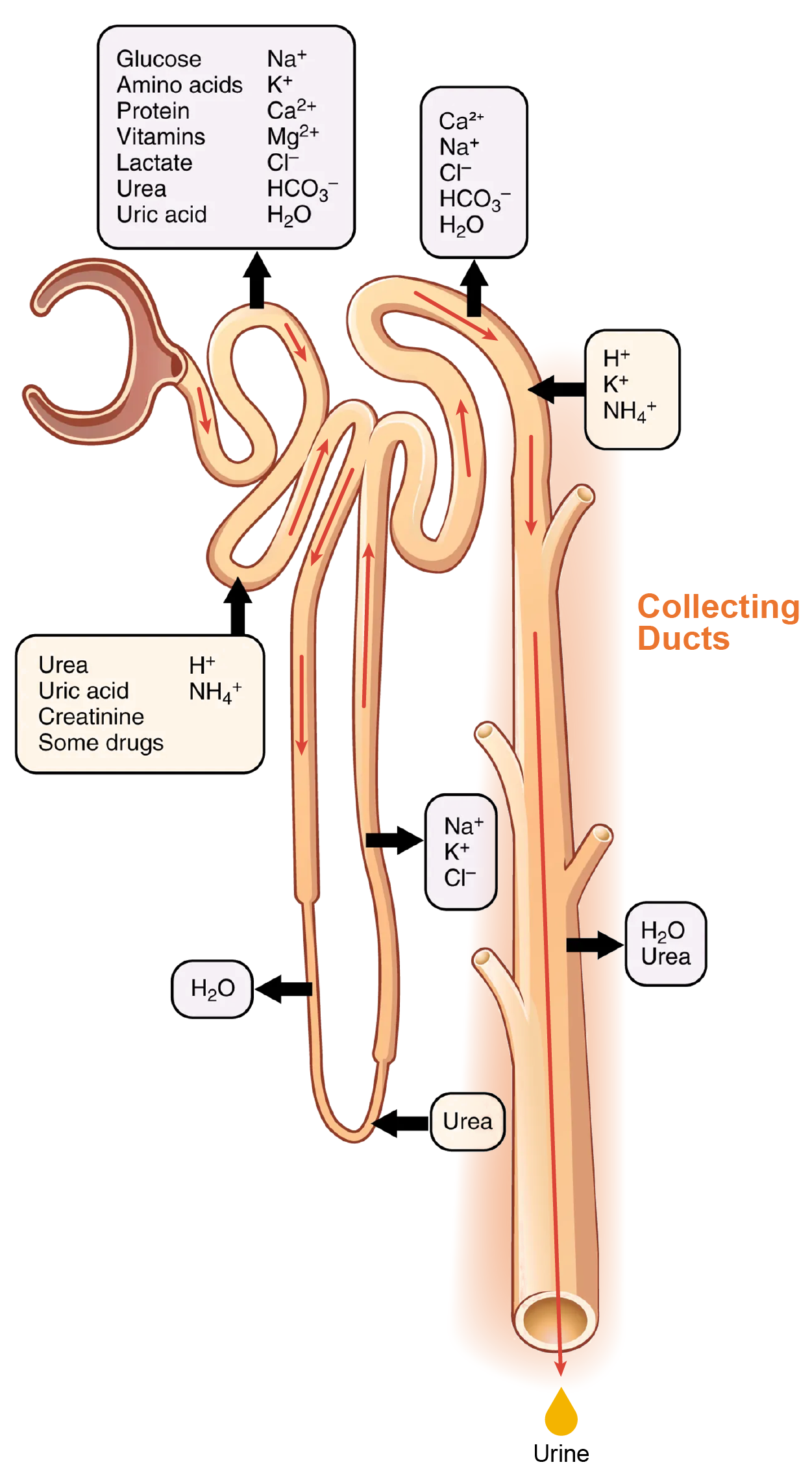
What is happening in late DCT and collecting ducts:
This function is regulated by the posterior pituitary hormone ADH (vasopressin). With mild dehydration, plasma osmolarity rises slightly. This increase is detected by osmoreceptors in the hypothalamus, which stimulates the release of ADH from the posterior pituitary. If plasma osmolarity decreases slightly, the opposite occurs.
When stimulated by ADH, aquaporin channels are inserted into the apical membrane of principal cells, which line the collecting ducts. As the ducts descend through the medulla, the osmolarity surrounding them increases (due to the countercurrent mechanisms described above). If aquaporin water channels are present, water will be osmotically pulled from the collecting duct into the surrounding interstitial space and into the peritubular capillaries. Therefore, the final urine will be more concentrated.
 Investigate the urinary system in three dimensions using augmented reality (AR)!
Investigate the urinary system in three dimensions using augmented reality (AR)!
SOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION. LICENSE: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.