Table of Contents |
The hypothalamus-pituitary complex can be thought of as the “command center” of the endocrine system. This complex secretes several hormones that directly produce responses in target tissues, as well as hormones that regulate the synthesis and secretion of hormones of other glands. In addition, the hypothalamus-pituitary complex coordinates the messages of the endocrine and nervous systems. In many cases, a stimulus received by the nervous system must pass through the hypothalamus-pituitary complex to be translated into hormones that can initiate a response.
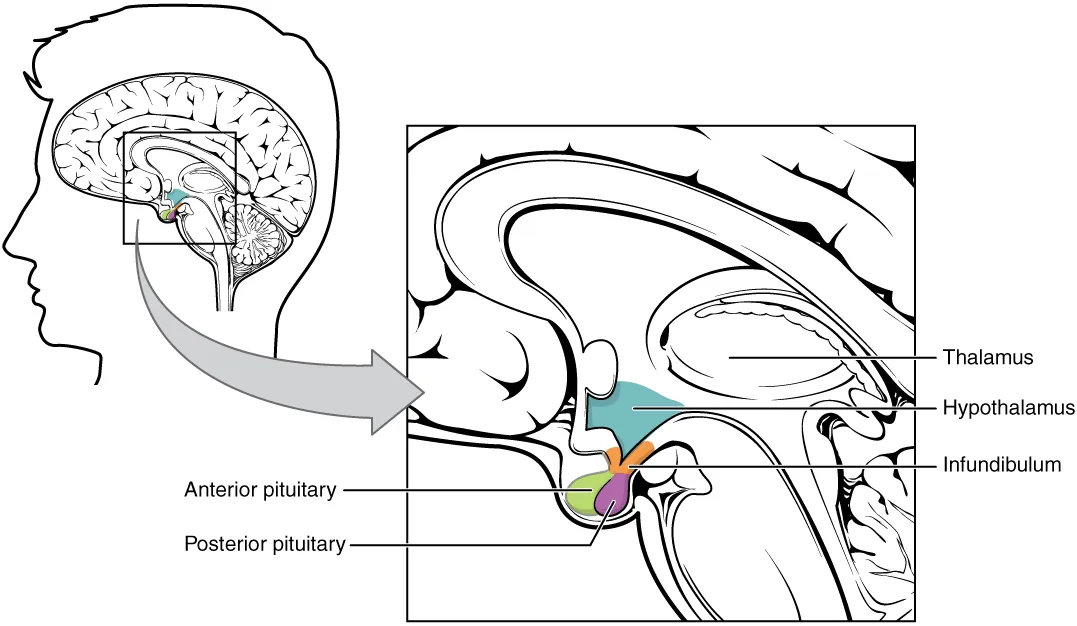
The hypothalamus is a structure of the diencephalon of the brain, which you may recall is located anterior and inferior to the thalamus. It has both neural and endocrine functions, producing and secreting many hormones. In addition, the hypothalamus is anatomically and functionally related to the pituitary gland (or hypophysis), a bean-sized organ suspended from it by a stem called the infundibulum (of the pituitary gland), or pituitary stalk.
The pituitary gland is cradled within the sella turcica of the sphenoid bone of the skull. It consists of two lobes that arise from distinct parts of embryonic tissue: The posterior pituitary (neurohypophysis) is neural tissue, whereas the anterior pituitary (also known as the adenohypophysis) is glandular tissue that develops from the primitive digestive tract.
Above, you learned about the structure and function of the hypothalamus-pituitary complex. Here, you will learn about more fine scale anatomical details of these organs and the hormones secreted by the hypothalamus and pituitary gland.
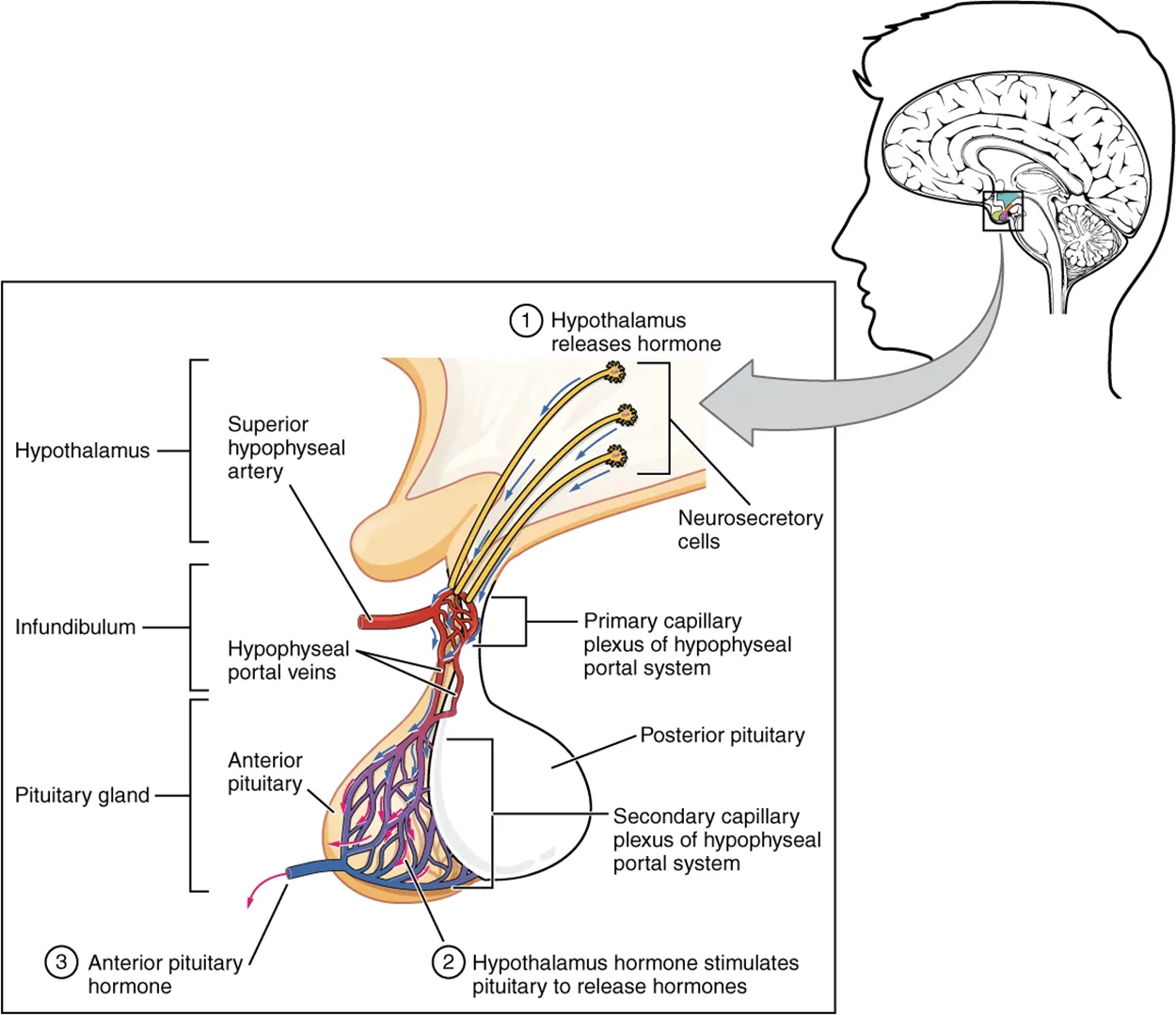
Hypothalamic hormones are secreted by neurons, but they enter the anterior pituitary through blood vessels. Within the infundibulum is a bridge of capillaries that connects the hypothalamus to the anterior pituitary. This network, called the hypophyseal portal system, allows hypothalamic hormones to be transported to the anterior pituitary without first entering the systemic circulation. This system originates from the superior hypophyseal artery, which branches off the carotid arteries and transports blood to the hypothalamus. The branches of the superior hypophyseal artery form the hypophyseal portal system.
Hypothalamic releasing and inhibiting hormones travel through a primary capillary plexus to the portal veins, which carry them into the anterior pituitary. Releasing hormones stimulate the release of hormones from the anterior and posterior pituitary, whereas inhibiting hormones inhibit hormone release. Hormones produced by the anterior pituitary (in response to releasing hormones) enter a secondary capillary plexus, and from there drain into the bloodstream.
| Hypothalamic Hormones | |
|---|---|
| Releasing and inhibiting hormones |
Oxytocin plays a couple of different roles. One of its targets are mammary glands, which cause milk to move into the ducts during breastfeeding. Oxytocin also acts on muscles within uterine walls, causing contractions during childbirth. Essentially, oxytocin levels rise when a woman needs to give birth and is what causes labor contractions and pains. In summary, oxytocin acts on mammary glands to move milk into ducts and to help with contractions during childbirth. |
| Antidiuretic hormone (ADH) | Antidiuretic hormone causes water to be conserved within kidney nephrons, lowering someone's urine output. |
| Somatostatin (or growth hormone-inhibiting hormone (GHIH)) | Somatostatin inhibits the secretion of human growth hormone. |
The posterior pituitary is actually an extension of the neurons of the paraventricular and supraoptic nuclei of the hypothalamus. The cell bodies of these regions rest in the hypothalamus, but their axons descend as the hypothalamic–hypophyseal tract within the infundibulum and end in axon terminals that comprise the posterior pituitary.
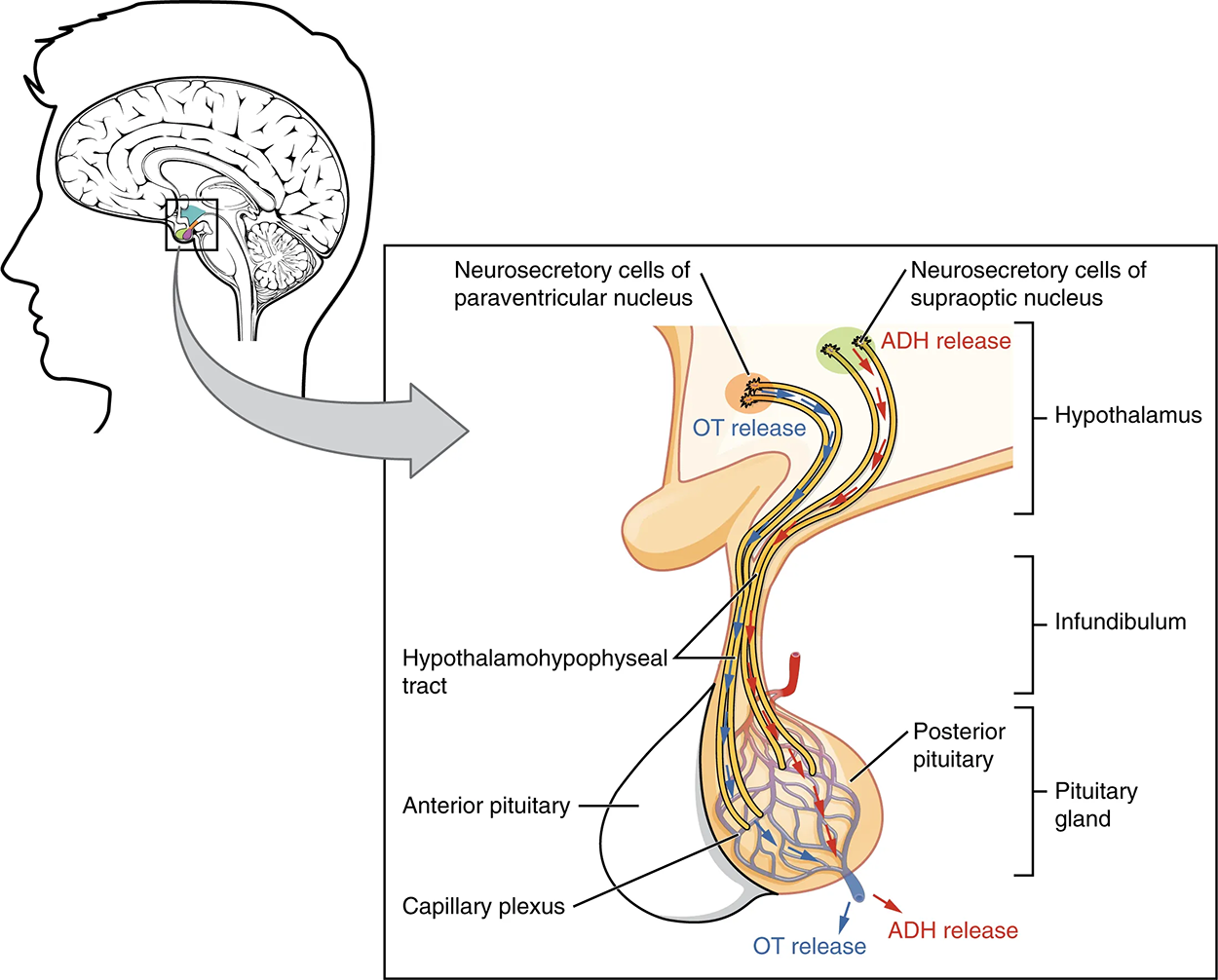
Below are two hormones that are produced by the posterior pituitary.
| Posterior Pituitary Hormones | |
|---|---|
| Oxytocin |
Oxytocin plays a couple of different roles. One of its targets are mammary glands, which cause milk to move into the ducts during breastfeeding. Oxytocin also acts on muscles within uterine walls, causing contractions during childbirth. Essentially, oxytocin levels rise when a woman needs to give birth and is what causes labor contractions and pains. In summary, oxytocin acts on mammary glands to move milk into ducts and to help with contractions during childbirth. |
| Antidiuretic hormone (ADH) | Antidiuretic hormone causes water to be conserved within kidney nephrons, lowering someone's urine output. |
Recall that the posterior pituitary does not synthesize hormones, but merely stores them. In contrast, the anterior pituitary does manufacture hormones. However, the secretion of hormones from the anterior pituitary is regulated by two classes of hormones. These hormones—secreted by the hypothalamus—are the releasing hormones that stimulate the secretion of hormones from the anterior pituitary and the inhibiting hormones that inhibit secretion.
The anterior pituitary produces seven hormones. These include:
| Anterior Pituitary Hormones | |
|---|---|
| Prolactin (PRL) | A hormone that plays a role in milk production in mammary glands. |
| Luteinizing hormone (LH) | A hormone that plays a role in the reproductive system. It also helps with the secretion of other hormones and targets mostly in the ovaries and testes. |
| Follicle-stimulating hormone (FSH) | Another hormone that plays a role in the reproductive system; it targets the ovaries and testes, and it plays a role in egg and sperm. |
| Thyroid-stimulating hormone (TSH) | A hormone that controls the release of thyroid hormone. |
| Adrenocorticotropic hormone (ACTH) | A hormone that stimulates the release of cortisol from the adrenal glands. |
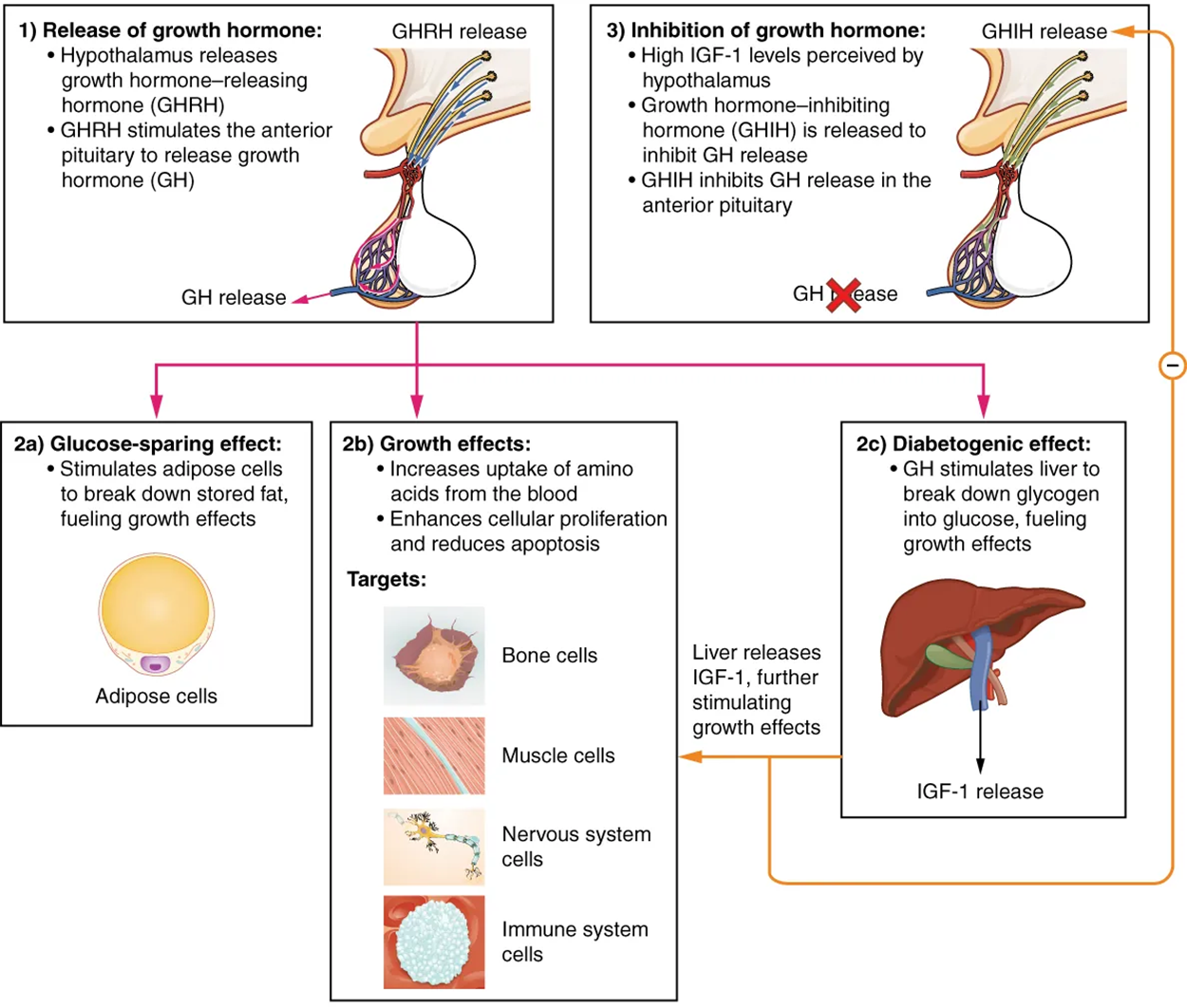
| Growth hormone (GH) | A hormone that regulates a person's growth that is secreted by this anterior lobe. |
| Beta endorphin | A hormone that is involved in functions such as managing pain, stress reduction, and your reward circuitry. |
GH is a well-known hormone of the anterior pituitary. The figure below describes how GH helps regulate growth.
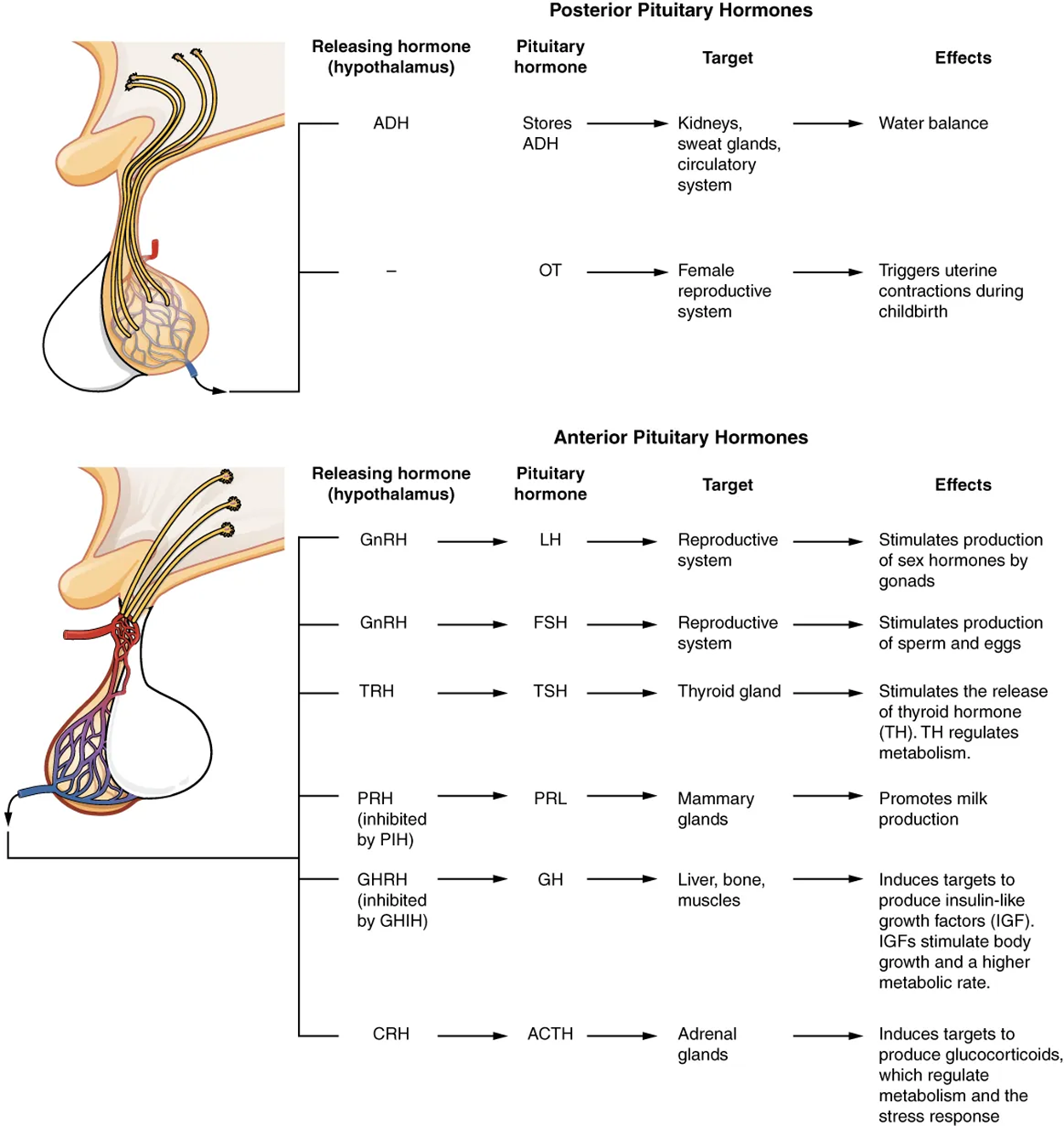
The figure below summarizes some of the major hormones of the posterior and anterior pituitary, their targets, and the effects they have on their targets.
The cells in the zone between the pituitary lobes secrete a hormone known as melanocyte-stimulating hormone (MSH) that is formed by cleavage of the pro-opiomelanocortin (POMC) precursor protein. Local production of MSH in the skin is responsible for melanin production in response to UV light exposure.
However, the role of MSH made by the pituitary is more complicated. For instance, people with lighter skin generally have the same amount of MSH as people with darker skin. Nevertheless, this hormone is capable of darkening the skin by inducing melanin production in the skin’s melanocytes. People also show increased MSH production during pregnancy; in combination with estrogens, it can lead to darker skin pigmentation, especially the skin of the areolas and labia minora.
Recall that the hypothalamus, part of the diencephalon of the brain, sits inferior and somewhat anterior to the thalamus. Inferior but somewhat posterior to the thalamus is the pineal gland, a tiny endocrine gland whose functions are not entirely clear. However, the pinealocyte cells that make up the pineal gland are known to produce and secrete the amine hormone melatonin, which is derived from serotonin.
The rate of melatonin production is affected by the photoperiod. Collaterals from the visual pathways innervate the pineal gland. During the day photoperiod, little melatonin is produced; however, melatonin production increases during the dark photoperiod (night). In some mammals, melatonin has an inhibitory effect on reproductive functions by decreasing production and maturation of sperm, oocytes, and reproductive organs. Melatonin is an effective antioxidant, protecting the CNS from free radicals such as nitric oxide and hydrogen peroxide. Lastly, melatonin is involved in biological rhythms, particularly circadian rhythms such as the sleep–wake cycle and eating habits.
The secretion of melatonin varies according to the level of light received from the environment. When photons of light stimulate the retinas of the eyes, a nerve impulse is sent to a region of the hypothalamus called the suprachiasmatic nucleus (SCN), which is important in regulating biological rhythms. From the SCN, the nerve signal is carried to the spinal cord and eventually to the pineal gland, where the production of melatonin is inhibited. As a result, blood levels of melatonin fall, promoting wakefulness. In contrast, as light levels decline—such as during the evening—melatonin production increases, boosting blood levels and causing drowsiness.
The secretion of melatonin may influence the body’s circadian rhythms, which are the light–dark fluctuations that affect not only sleepiness and wakefulness, but also appetite and body temperature. Interestingly, children have higher melatonin levels than adults, which may prevent the release of gonadotropins from the anterior pituitary, thereby inhibiting the onset of puberty. Finally, there is an antioxidant role of melatonin.
SOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION. LICENSE: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.