Table of Contents |
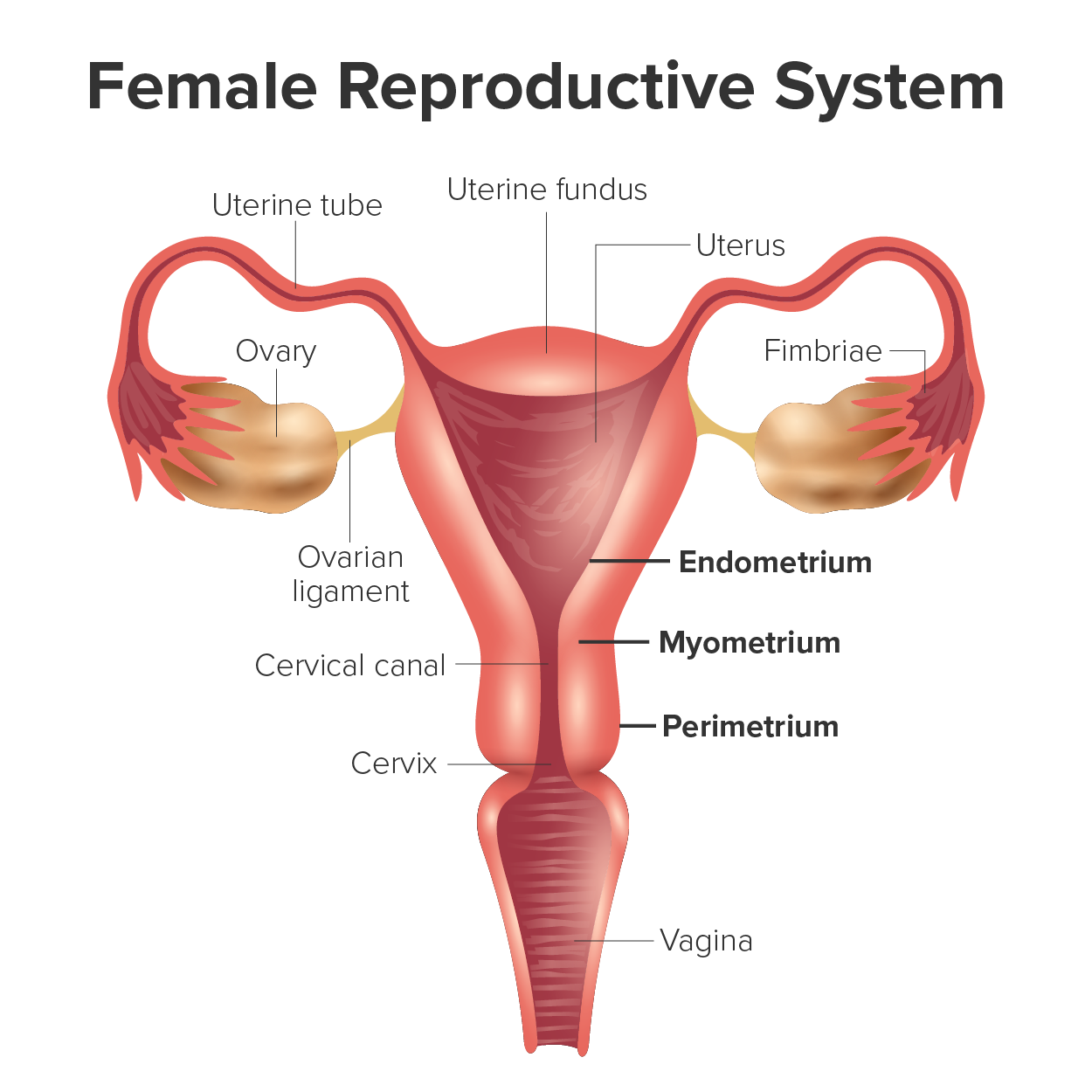
The wall of the uterus is made up of three layers that play important roles in the uterine cycle, which you will learn more about later in this lesson.
Structurally, the endometrium consists of two layers: the stratum basalis and the stratum functionalis (the basal and functional layers). The stratum basalis layer is part of the lamina propria and is adjacent to the myometrium; this layer is not shed during menses. In contrast, the thicker stratum functionalis layer contains the glandular portion of the lamina propria and the endothelial tissue that lines the uterine lumen. It is the stratum functionalis that grows and thickens in response to increased levels of estrogen and progesterone. In the luteal phase of the uterine cycle, special branches from the uterine artery called spiral arteries supply the thickened stratum functionalis. This inner functional layer provides the proper site of implantation for the fertilized egg, and—should fertilization not occur—it is only the stratum functionalis layer of the endometrium that sheds during menstruation.
Recall that, during the follicular phase of the ovarian cycle, the tertiary follicles are growing and secreting estrogen. At the same time, the stratum functionalis of the endometrium is thickening to prepare for a potential implantation. The post-ovulatory increase in progesterone, which you will learn characterizes the luteal phase, is key for maintaining a thick stratum functionalis. As long as a functional corpus luteum is present in the ovary, the endometrial lining is prepared for implantation.
Indeed, if an embryo implants, signals are sent to the corpus luteum (a transformed follicle that forms after ovulation and secretes progesterone) to continue secreting progesterone to maintain the endometrium, and thus maintain the pregnancy. If an embryo does not implant, no signal is sent to the corpus luteum and it degrades, ceasing progesterone production and ending the luteal phase. Without progesterone, the endometrium thins and, under the influence of prostaglandins, the spiral arteries of the endometrium constrict and rupture, preventing oxygenated blood from reaching the endometrial tissue. As a result, endometrial tissue dies and blood, pieces of the endometrial tissue, and white blood cells are shed through the vagina during menstruation, or the menses. The first menses after puberty, called menarche, can occur either before or after the first ovulation.
EXAMPLE
| Term | Pronunciation | Audio File |
|---|---|---|
| Perimetrium | peri·me·tri·um |
|
| Myometrium | myo·me·tri·um |
|
| Endometrium | en·do·me·tri·um |
|
| Menses | men·ses |
|
| Menarche | men·ar·che |
|
Now that we have discussed the maturation of the cohort of tertiary follicles in the ovary, the build-up and then shedding of the endometrial lining in the uterus, and the function of the uterine tubes and vagina, we can put everything together to talk about the three phases of the uterine cycle (also known as the menstrual cycle)—the series of changes in which the uterine lining is shed, rebuilds, and prepares for implantation.
The timing of the uterine cycle starts with the first day of menses, which is referred to as day one of a period. Cycle length is determined by counting the days between the onset of bleeding in two subsequent cycles. Because the average length of a uterine cycle is 28 days, this is the time period used to identify the timing of events in the cycle. The length of the uterine cycle varies even in the same person from one cycle to the next, typically from 21 to 32 days. However, in all instances, there are three phases of the uterine cycle: the menses phase, the proliferative phase, and the secretory phase.
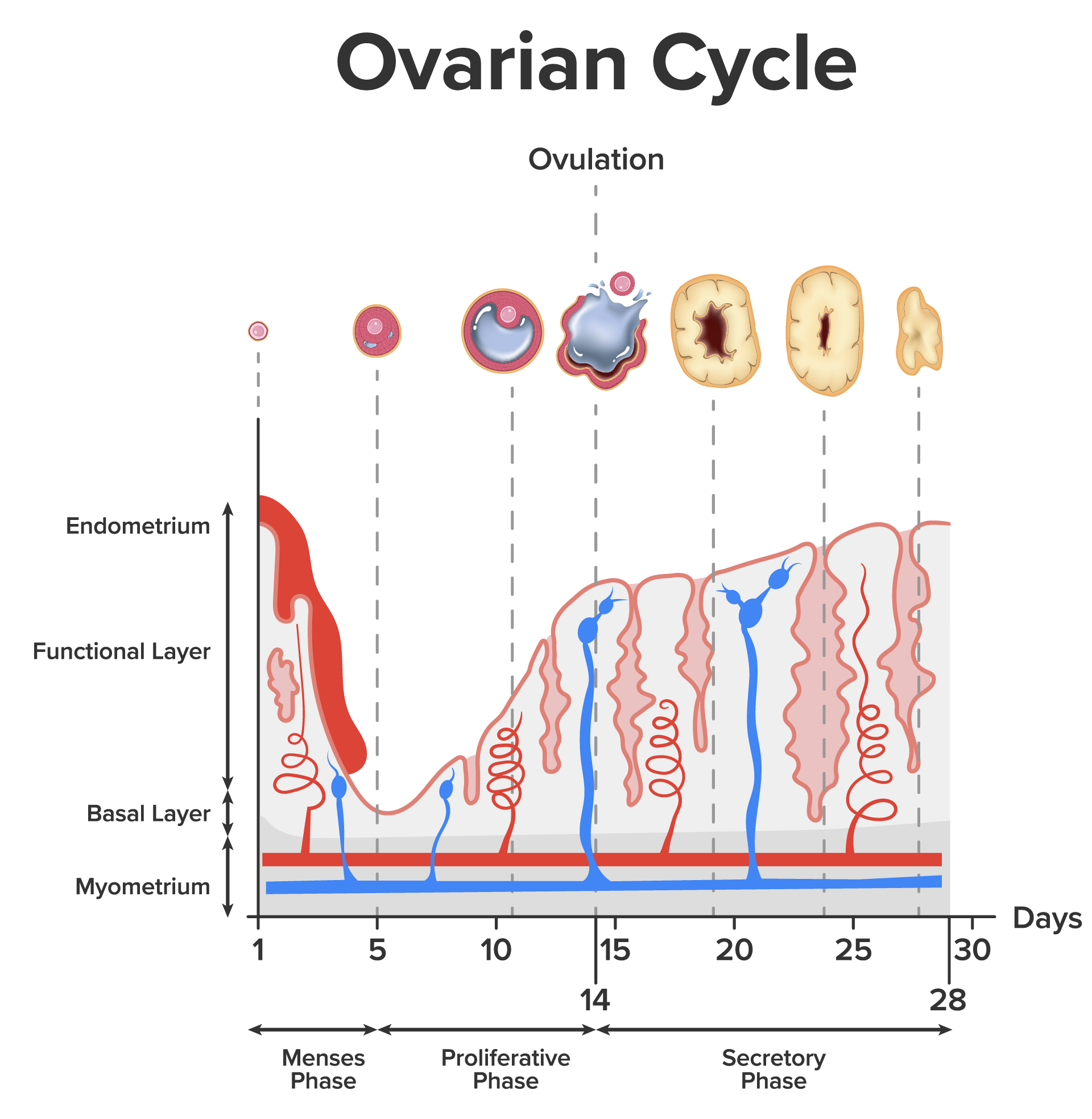
The menses phase (also known as the menstrual phase) of the uterine cycle is the phase during which the lining is shed; that is, the days that the person menstruates. Although it averages approximately 5 days, the menses phase can last from 2 to 7 days, or longer.
Once menstrual flow ceases, the endometrium begins to proliferate again, marking the beginning of the proliferative phase of the uterine cycle. This is the phase where the endometrium proliferates. In a typical 28-day uterine cycle, ovulation occurs on day 14. Ovulation marks the end of the proliferative phase in the uterine cycle as well as the end of the follicular phase in the ovarian cycle.
In the uterus, progesterone from the corpus luteum begins the secretory phase of the uterine cycle, in which the endometrial lining prepares for implantation. Over the next 10 to 12 days, the endometrial glands secrete a fluid rich in glycogen. If fertilization has occurred, this fluid will nourish the ball of cells now developing from the zygote. At the same time, the spiral arteries develop to provide blood to the thickened stratum functionalis.
If no pregnancy occurs within approximately 10 to 12 days, the corpus luteum will degrade into the corpus albicans, which is a nonfunctional structure that disintegrates over time. The endometrial tissue will die, resulting in menses—or the first day of the next cycle.
| Term | Pronunciation | Audio File |
|---|---|---|
| Proliferative Phase | pro·lif·er·ate ph·ase |
|
| Secretory Phase | se·cre·to·ry ph·ase |
|
Source: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX "ANATOMY AND PHYSIOLOGY 2E" ACCESS FOR FREE AT OPENSTAX.ORG/DETAILS/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E. LICENSE: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL
REFERENCES
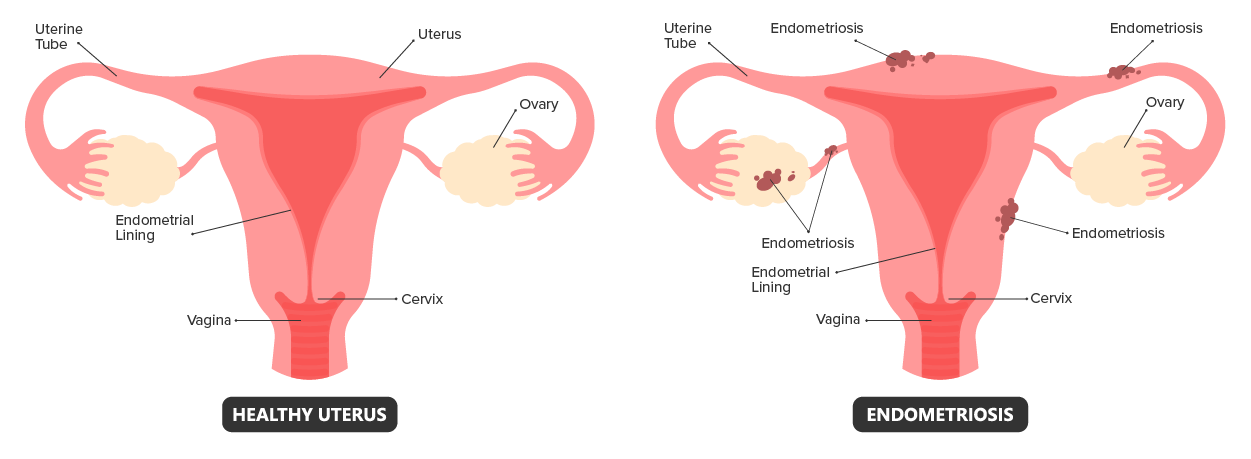
National Institutes of Health. "What are the treatments for endometriosis?". Retrieved November 1, 2023, from www.nichd.nih.gov/health/topics/endometri/conditioninfo/treatment
Mayo Clinic. "Endometriosis". Retrieved November 1, 2023, from www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656