Table of Contents |
Communication is a process in which a sender transmits signals to one or more receivers to control and coordinate actions. In the human body, two major organ systems participate in relatively “long distance” communication: the nervous system, which uses electrical signaling, and the endocrine system, which uses chemical signaling. Together, these two systems are primarily responsible for maintaining homeostasis in the body.
The endocrine system in particular has many essential roles in the human body, such as maintaining blood sugar; differentiation, growth, and function of reproductive organs; body growth; and energy production.
The endocrine system produces chemicals called hormones that function to control and regulate many different body processes. Hormones are released into body fluids, usually blood, which carries them to their target cells where they elicit a response. The cells that secrete hormones are often located in specific organs, called endocrine glands, and the cells, tissues, and organs that secrete hormones make up the endocrine system. Examples of endocrine organs include the pancreas, which produces the hormones insulin and glucagon to regulate blood glucose levels; the adrenal glands, which produce hormones such as epinephrine and norepinephrine that regulate responses to stress; and the thyroid gland, which produces thyroid hormones that regulate metabolic rates.
The endocrine system consists of cells, tissues, and organs that secrete hormones as a primary or secondary function. The endocrine gland is the major player in this system. The primary function of these ductless glands is to secrete their hormones directly into the surrounding fluid. The interstitial fluid and the blood vessels then transport the hormones throughout the body.
The endocrine system includes the pituitary, thyroid, parathyroid, adrenal, and pineal glands, whose primary functions are as endocrine glands that secrete hormones. However, some components of the endocrine system have both endocrine and non-endocrine functions.
EXAMPLE
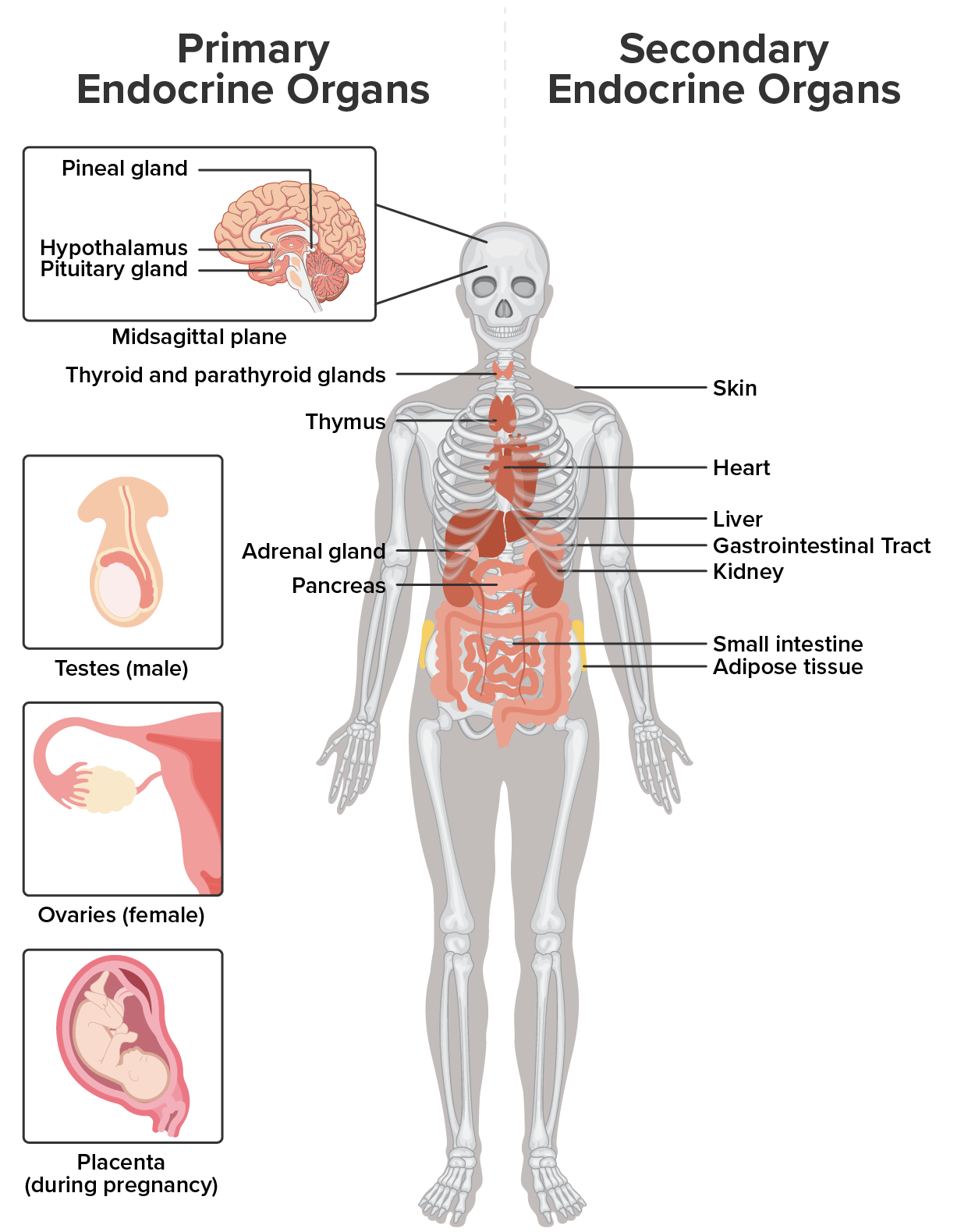
As you learned earlier in this lesson, the pancreas contains cells that function in digestion as well as cells that secrete the hormones insulin and glucagon, which regulate blood glucose levels. The hypothalamus, thymus, heart, kidneys, stomach, small intestine, liver, skin, ovaries, and testes are other organs that contain cells with endocrine function. Moreover, adipose tissue has long been known to produce hormones, and recent research has revealed that even bone tissue has endocrine functions.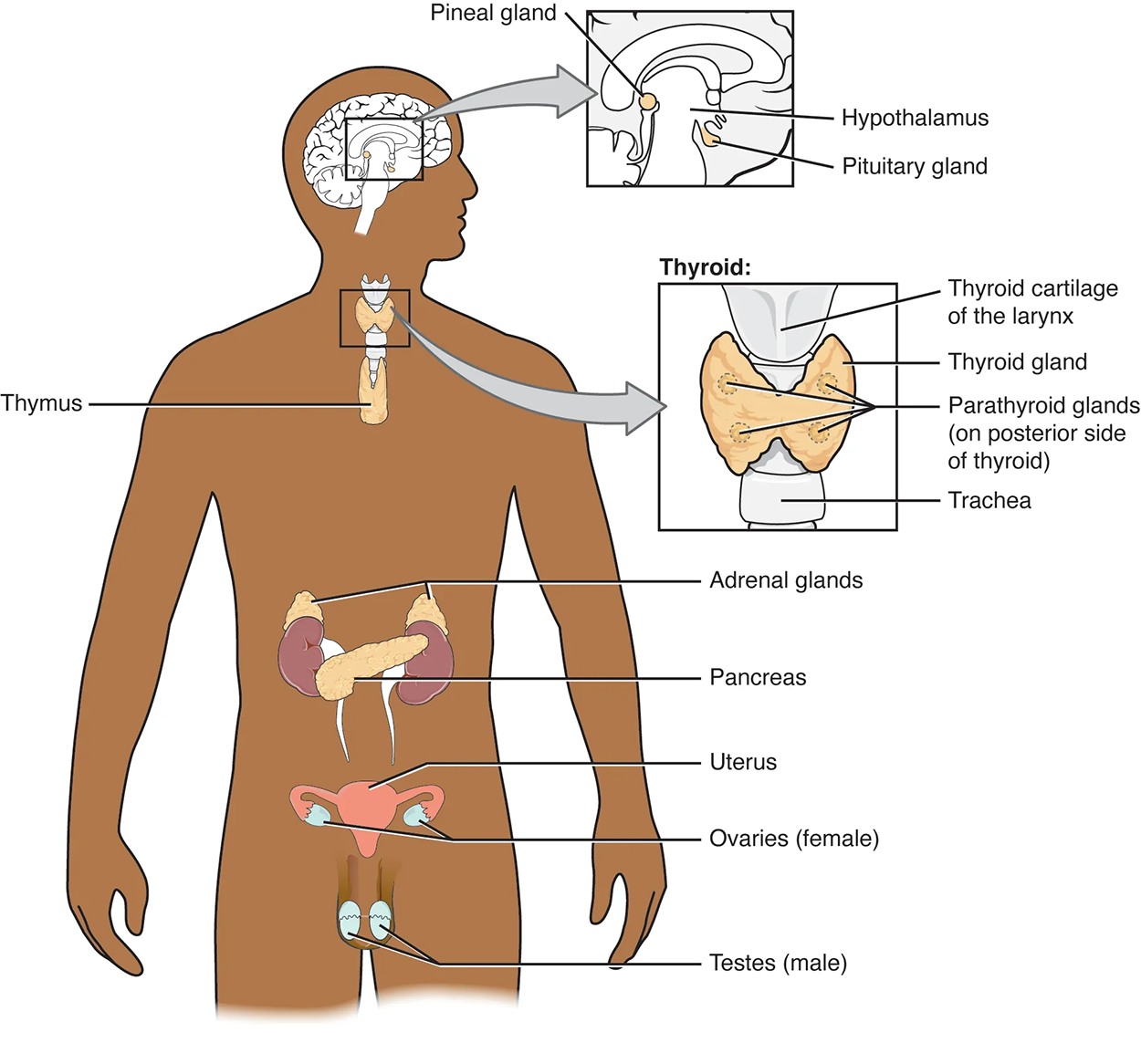
The ductless endocrine glands are not to be confused with the body’s exocrine system, whose glands release their secretions through ducts. Examples of exocrine glands include the sebaceous and sweat glands of the skin. As just noted, the pancreas also has an exocrine function: Most of its cells secrete pancreatic juice through the pancreatic and accessory ducts to the lumen of the small intestine.
As noted above, there are two types of endocrine organs: primary and secondary.
The table below describes the primary endocrine glands, associated hormones, and their effects. You will learn more about these organs in future lessons.
| Endocrine Glands and Their Associated Hormones | ||
|---|---|---|
| Endocrine Gland | Associated Hormones | Effect |
| Hypothalamus | ||
| Releasing and inhibiting hormones | Regulate hormone release from pituitary gland; produce oxytocin; produce uterine contractions and milk secretion in breast tissue | |
| Antidiuretic hormone (ADH) (produced) | Water reabsorption from kidneys; vasoconstriction to increase blood pressure | |
| Somatostatin (or growth hormone-inhibiting hormone (GHIH)) | Inhibit secretion of human growth hormone | |
| Pituitary (Anterior) | ||
| Growth hormone (GH) | Promote growth of body tissues, protein synthesis; metabolic functions | |
| Prolactin (PRL) | Promote milk production | |
| Thyroid-stimulating hormone (TSH) | Stimulate thyroid hormone release | |
| Adrenocorticotropic hormone (ACTH) | Stimulate hormone release by adrenal cortex, glucocorticoids | |
| Follicle-stimulating hormone (FSH) | Stimulate gamete production (both ova and sperm); secretion of estradiol | |
| Luteinizing hormone (LH) | Stimulate androgen production by gonads; ovulation, secretion of progesterone | |
| Melanocyte-stimulating hormone (MSH) | Stimulate melanocytes of the skin, increasing melanin pigment production | |
| Pituitary (Posterior) | ||
| Antidiuretic hormone (ADH) (storage) | Stimulate water reabsorption by kidneys | |
| Oxytocin | Stimulate uterine contractions during childbirth; milk ejection; stimulate ductus deferens and prostate gland contraction during emission | |
| Thyroid | ||
| Thyroxine (T₄), Triiodothyronine (T₃) | Stimulate and maintain metabolism; growth and development | |
| Calcitonin | Reduce blood Ca²⁺ levels | |
| Parathyroid | Parathyroid hormone (PTH) | Increase blood Ca²⁺ levels |
| Adrenal (Cortex) | ||
| Aldosterone | Increase blood Na⁺ levels; increase K⁺ secretion | |
| Cortisol, Corticosterone, Cortisone | Increase blood glucose levels; anti-inflammatory effects | |
| Androgens | Sex hormones produced during puberty and most of adulthood; supplement gonadal androgens | |
| Adrenal (Medulla) | Epinephrine, Norepinephrine | Stimulate fight-or-flight response; increase blood glucose levels; increase metabolic activities |
| Pancreas | ||
| Insulin | Reduce blood glucose levels | |
| Glucagon | Increase blood glucose levels | |
| Somatostatin (or growth hormone-inhibiting hormone (GHIH)) | Inhibit secretion of human growth hormone | |
| Pineal gland | Melatonin | Regulate some biological rhythms and protect CNS from free radicals |
| Testes | Androgens | Regulate, promote, increase, or maintain sperm production; a suite of characteristics including growth and development of the testes and penis, increased skeletal and muscular growth, enlargement of the larynx, and increased growth and redistribution of body hair |
| Ovaries | ||
| Estrogen | Promote uterine lining growth; a suite of characteristics including increased development of breast tissue, redistribution of fat towards hips, legs, and breast, and the maturation of the uterus and vagina | |
| Progestins | Promote and maintain uterine lining growth | |
IN CONTEXT
Career Connection: Endocrinologist
Endocrinology is a specialty in the field of medicine that focuses on the treatment of endocrine system disorders. Endocrinologists—medical doctors who specialize in this field—are experts in treating diseases associated with hormonal systems, ranging from thyroid disease to diabetes mellitus. Endocrine surgeons treat endocrine disease through the removal, or resection, of the affected endocrine gland.
Patients who are referred to endocrinologists may have signs and symptoms or blood test results that suggest excessive or impaired functioning of an endocrine gland or endocrine cells. The endocrinologist may order additional blood tests to determine whether the patient’s hormonal levels are abnormal, or they may stimulate or suppress the function of the suspect endocrine gland and then have blood taken for analysis.
Treatment varies according to the diagnosis. Some endocrine disorders, such as type 2 diabetes, may respond to lifestyle changes such as modest weight loss, adoption of a healthy diet, and regular physical activity. Other disorders may require medication, such as hormone replacement, and routine monitoring by the endocrinologist. These include disorders of the pituitary gland that can affect growth and disorders of the thyroid gland that can result in a variety of metabolic problems.
Some patients experience health problems as a result of the normal decline in hormones that can accompany aging. These patients can consult with an endocrinologist to weigh the risks and benefits of hormone replacement therapy intended to boost their natural levels of reproductive hormones.
In addition to treating patients, endocrinologists may be involved in research to improve the understanding of endocrine system disorders and develop new treatments for these diseases.
There are several organs whose primary functions are non-endocrine but that also possess endocrine functions. These include the heart, kidneys, intestines, thymus, gonads, and adipose tissue.
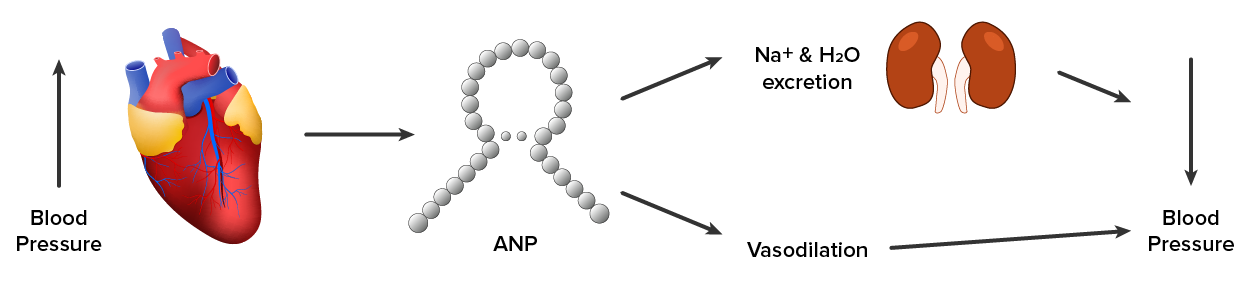
The heart possesses endocrine cells that are specialized cardiac muscle cells. These cells release the hormone atrial natriuretic peptide (ANP) in response to increased blood volume. High blood volume causes the cells to be stretched, resulting in hormone release. ANP acts on the kidneys to reduce the reabsorption of sodium (Na⁺), causing Na⁺ and water to be excreted in the urine. ANP also reduces the amounts of renin released by the kidneys and aldosterone released by the adrenal cortex, further preventing the retention of water. In this way, ANP causes a reduction in blood volume and blood pressure and reduces the concentration of Na⁺ in the blood.
The gastrointestinal tract produces several hormones that aid in digestion. The endocrine cells are located in the mucosa of the GI tract throughout the stomach and small intestine. Some of the hormones produced include gastrin, secretin, and cholecystokinin, which are secreted in the presence of food, and some of which act on other organs such as the pancreas, gallbladder, and liver. They trigger the release of gastric juices, which help to break down and digest food in the GI tract.
While the adrenal glands associated with the kidneys are major endocrine glands, the kidneys themselves also possess endocrine function. Renin is released in response to decreased blood volume or pressure and is part of the renin-angiotensin-aldosterone system that leads to the release of aldosterone. Aldosterone then causes the retention of Na⁺ and water, raising blood volume.
The kidneys also release calcitriol, which aids in the absorption of calcium (Ca²⁺) and phosphate ions. Erythropoietin (EPO) is a protein hormone that triggers the formation of red blood cells in the bone marrow. EPO is released in response to low oxygen levels. Because red blood cells are oxygen carriers, increased production results in greater oxygen delivery throughout the body.
The thymus is found behind the sternum; it is most prominent in infants, becoming smaller in size through adulthood. The thymus produces hormones referred to as thymosins, which contribute to the development of the immune response.
Adipose tissue is a connective tissue found throughout the body. It produces the hormone leptin in response to food intake. Leptin increases the activity of anorexigenic neurons and decreases that of orexigenic neurons, producing a feeling of satiety after eating, thus affecting appetite and reducing the urge for further eating. Leptin is also associated with reproduction. It must be present for GnRH and gonadotropin synthesis to occur. Extremely thin females may enter puberty late; however, if adipose levels increase, more leptin will be produced, improving fertility.
The liver is responsible for secreting at least four important hormones or hormone precursors: insulin-like growth factor (somatomedin), angiotensinogen, thrombopoietin, and hepcidin. Insulin-like growth factor-1 is the immediate stimulus for growth in the body, especially of the bones. Angiotensinogen is the precursor to angiotensin II, mentioned earlier, which increases blood pressure. Thrombopoietin stimulates the production of the blood’s platelets. Hepcidins block the release of iron from cells in the body, helping to regulate iron homeostasis in our body fluids.
IN CONTEXT
Thrombocytopenia refers to an insufficient number of platelets. Insufficient thrombopoietin levels can result in thrombocytopenia and may be caused by impaired production and/or increased destruction of thrombopoietin. A low platelet count can result in abnormal and excessive bleeding.
EXAMPLE
Individuals with thrombocytopenia may bruise easily, have cuts that bleed for prolonged periods, experience abnormal bleeding such as bleeding gums, and have purplish-red rashes from tiny spots of bleeding under the skin (petechiae).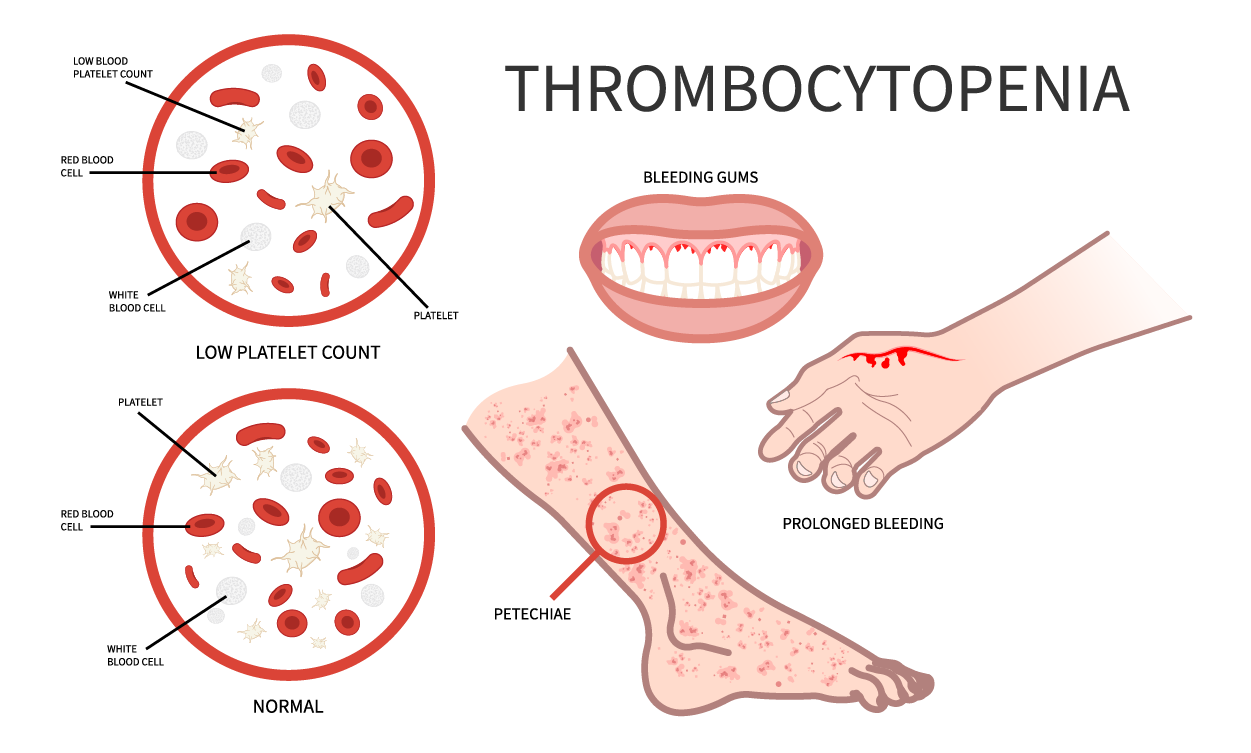
| Organs With Secondary Endocrine Functions and Their Major Hormones | ||
|---|---|---|
| Organ | Major hormones | Effects |
| Heart | Atrial natriuretic peptide (ANP) | Reduces blood volume, blood pressure, and Na⁺ concentration |
| Gastrointestinal tract | Gastrin, secretin, and cholecystokinin | Aids digestion of food and buffering of stomach acids |
| Gastrointestinal tract | Glucose-dependent insulinotropic peptide (GIP) and glucagon-like peptide 1 (GLP-1) | Stimulates beta cells of the pancreas to release insulin |
| Kidneys | Renin | Converts angiotensinogen into angiotensin I, which ultimately gets converted to angiotensin II that stimulates the release of aldosterone |
| Kidneys | Calcitriol | Aids in the absorption of Ca²⁺ |
| Kidneys | Erythropoietin | Triggers the formation of red blood cells in the bone marrow |
| Skeleton | FGF23 | Inhibits production of calcitriol and increases phosphate excretion |
| Skeleton | Osteocalcin | Increases insulin production |
| Adipose tissue | Leptin | Promotes satiety signals in the brain |
| Adipose tissue | Adiponectin | Reduces insulin resistance |
| Skin | Cholecalciferol | Modified to form vitamin D |
| Thymus (and other organs) | Thymosins | Among other things, aids in the development of T lymphocytes of the immune system |
| Liver | Insulin-like growth factor-1 | Stimulates bodily growth |
| Liver | Angiotensinogen | Precursor to angiotensin II, which raises blood pressure |
| Liver | Thrombopoietin | Causes increase in platelets |
| Liver | Hepcidin | Blocks release of iron into body fluids |
The hormones of the human body can be divided into two major groups on the basis of their chemical structure. Hormones derived from amino acids include amines, peptides, and proteins. Those derived from lipids include steroids. These chemical groups affect a hormone’s distribution, the type of receptors it binds to, and other aspects of its function.
| Amine, Peptide, Protein, and Steroid Hormone Structure | ||
|---|---|---|
| Hormone Class | Components | Example(s) |
| Amine Hormone | Amino acids with modified groups (e.g., norepinephrine’s carboxyl group is replaced with a benzene ring) |
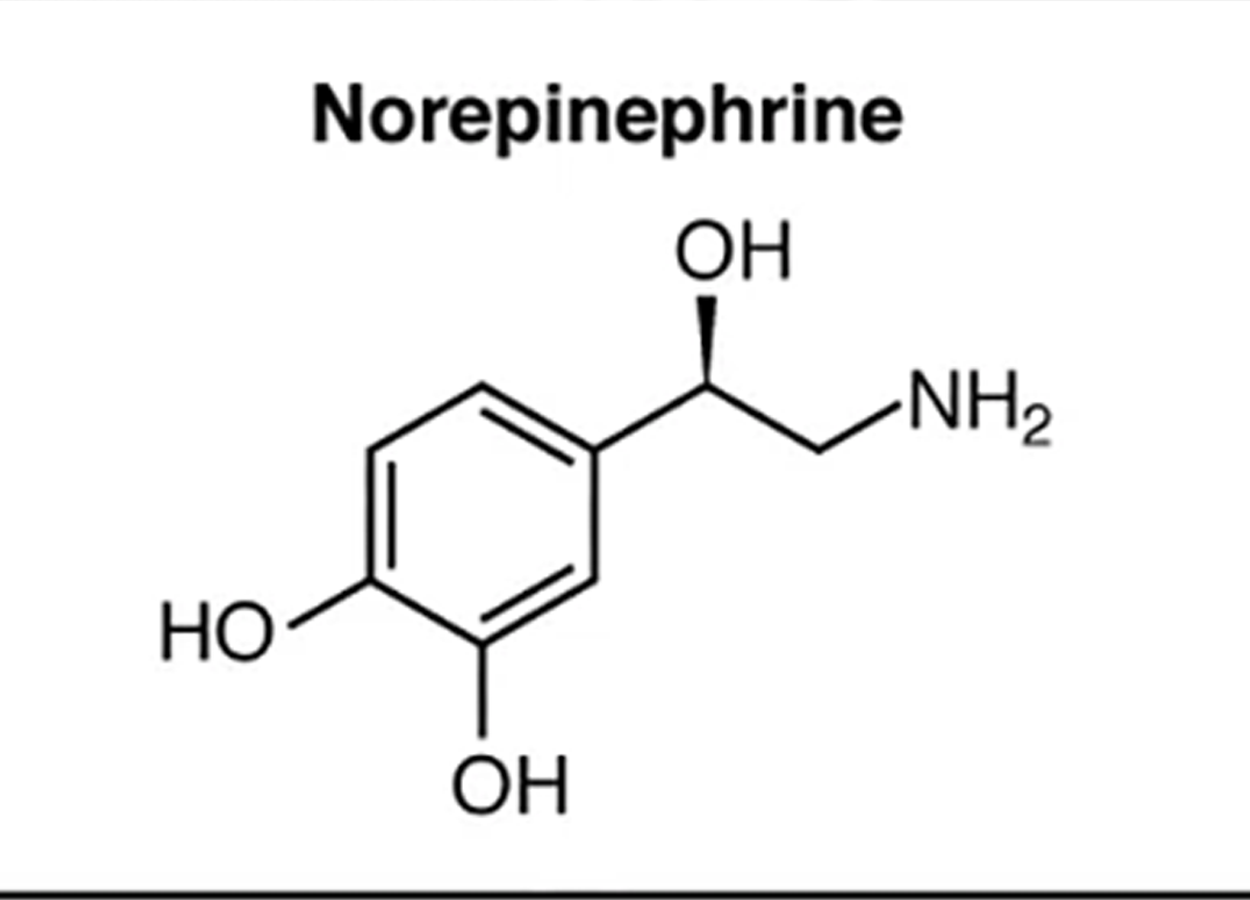
|
| Peptide Hormone | Short chains of linked amino acids |
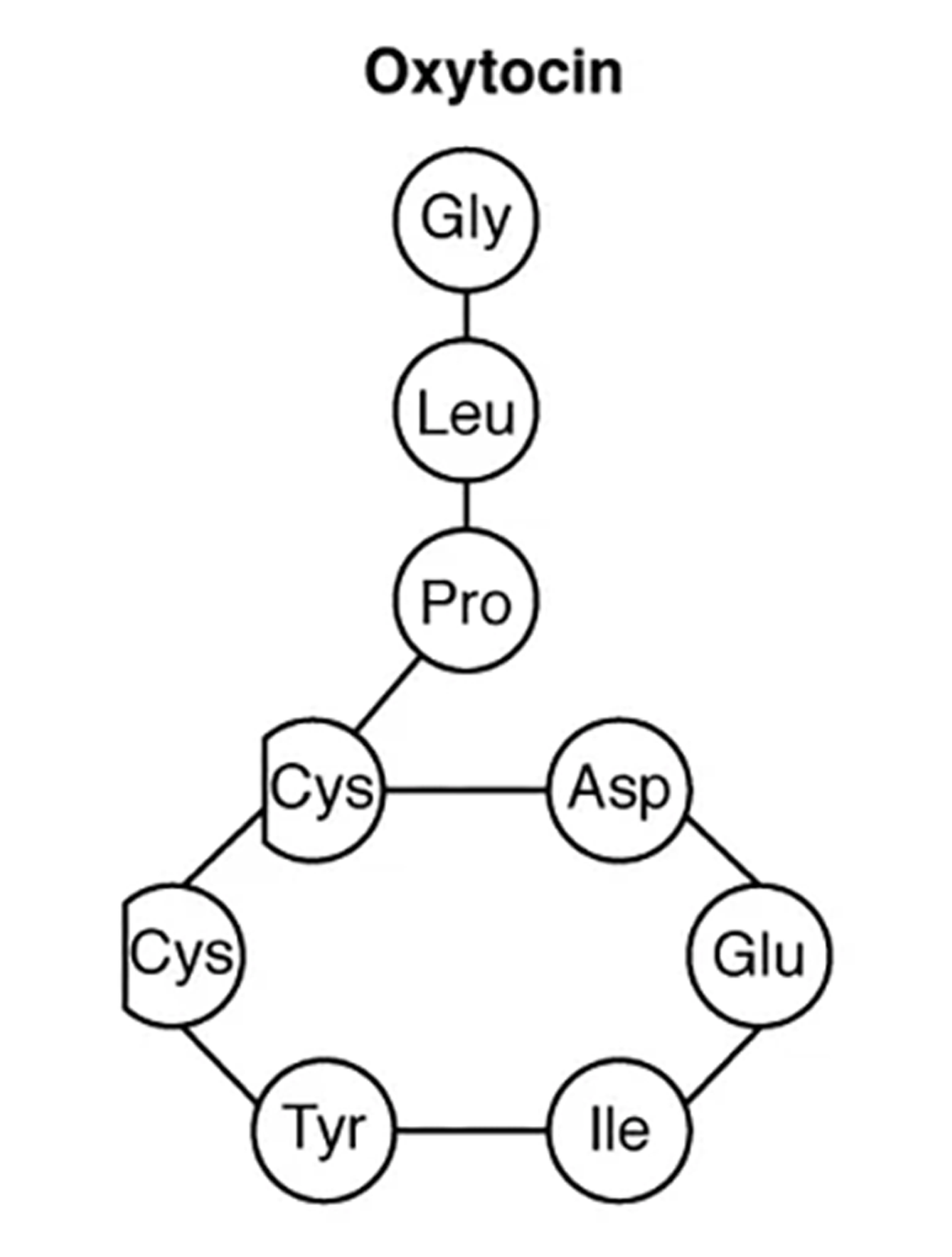
|
| Protein Hormone | Long chains of linked amino acids |
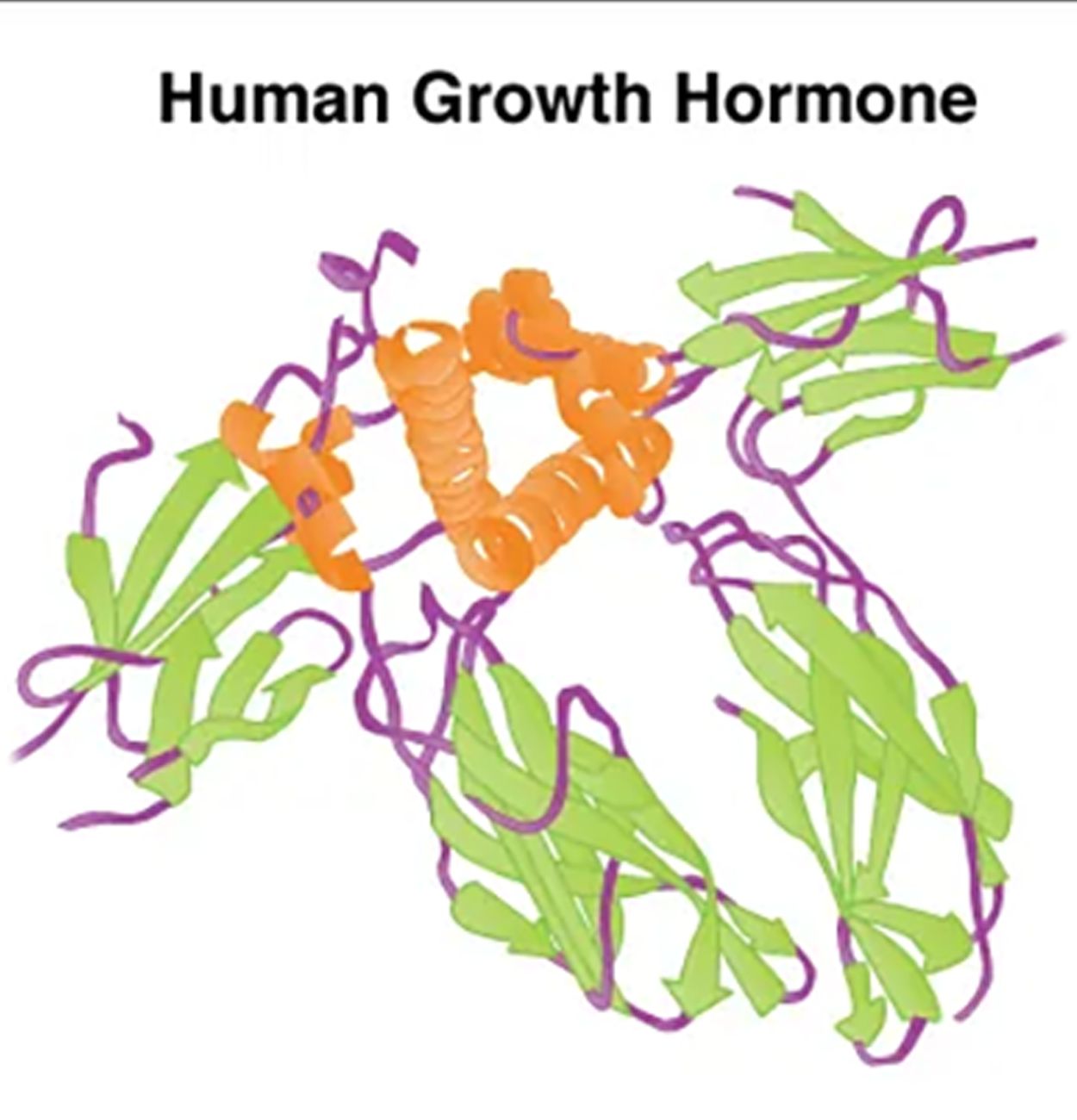
|
| Steroid Hormone | Derived from the lipid cholesterol |
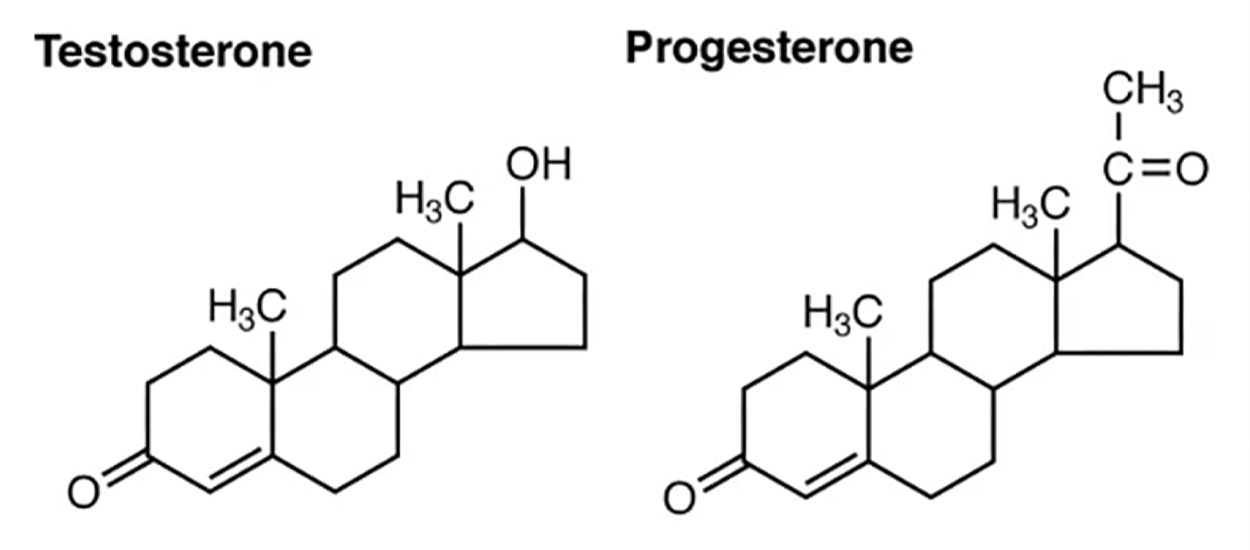
|
Amine hormones are synthesized from the amino acids tryptophan or tyrosine.
EXAMPLE
An example of a hormone derived from tryptophan is melatonin, which is secreted by the pineal gland and helps regulate circadian rhythm (your “internal clock” that helps regulate sleep and alertness).Tyrosine derivatives include the metabolism-regulating thyroid hormones as well as the catecholamines, such as epinephrine, norepinephrine, and dopamine. Epinephrine and norepinephrine are secreted by the adrenal medulla and play a role in the fight-or-flight response, whereas dopamine is secreted by the hypothalamus and inhibits the release of certain anterior pituitary hormones. Whereas the amine hormones are derived from a single amino acid, peptide and protein hormones consist of multiple amino acids that link to form an amino acid chain. Peptide hormones consist of short chains of amino acids, whereas protein hormones are longer polypeptides. Both types are synthesized like other body proteins: DNA is transcribed into mRNA, which is translated into an amino acid chain.
Examples of peptide hormones include antidiuretic hormone (ADH), a pituitary hormone important in fluid balance, and ANP, which you learned is produced by the heart and helps to decrease blood pressure.
EXAMPLE
Some examples of protein hormones include growth hormone, which is produced by the pituitary gland, and follicle-stimulating hormone (FSH), which has an attached carbohydrate group and is thus classified as a glycoprotein. FSH helps stimulate the maturation of eggs in the ovaries and sperm in the testes.The primary hormones derived from lipids are steroids. Steroid hormones are derived from the lipid cholesterol. For example, the reproductive hormones testosterone and the estrogens—which are produced by the gonads (testes and ovaries)—are steroid hormones. The adrenal glands produce the steroid hormone aldosterone, which is involved in osmoregulation (the control of salt and water balance across the membranes in the body’s fluids), and cortisol, which plays a role in metabolism.
Like cholesterol, steroid hormones are not soluble in water (they are hydrophobic). Because blood is water-based, lipid-derived hormones must bind to a transport protein to travel to their target cell. This more complex structure extends the half-life of steroid hormones, which is much longer than that of hormones derived from amino acids. A hormone’s half-life is the time required for half the concentration of the hormone to be degraded.
EXAMPLE
The lipid-derived hormone cortisol has a half-life of approximately 60 to 90 minutes. In contrast, the amino acid-derived hormone epinephrine has a half-life of approximately one minute. Interactive 3-D Model
Interactive 3-D ModelSOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM (1) OPENSTAX “BIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/BIOLOGY-2E/PAGES/1-INTRODUCTION (2) OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION. LICENSING (1 & 2): CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.