Table of Contents |
The concept of strategic planning has its roots in both political and military history. Many of the terms associated with strategic planning, such as “objectives,” “mission,” “strength,” and “weakness,” were developed by and used in the military (Zuckerman, 2016). Strategic planning in public health is a systematic process of envisioning a desired future and translating this vision into broadly defined goals or objectives and a sequence of steps to achieve them. In public health, this involves examining the entire spectrum of public health services and administration and optimizing care for all, operational efficiency, and organizational growth (American Journal of Healthcare Strategy, n.d.).
Strategic planning in public health is a process that helps organizations assess their environment, create a vision for the future, and develop a plan to achieve their goals. The resulting strategic plan is usually a formal document that guides the organization’s activities for several years. Strategic planning is an organization’s process of defining its strategy or direction. It involves making decisions on allocating resources to attain strategic goals and may extend to control mechanisms (e.g., tracking the progress of strategic initiatives; conducting evaluations to help ensure the program is on track; and monitoring continuous feedback from partners like the community, policymakers, or health care providers) for guiding strategy implementation.
 Some key aspects of strategic planning include defining strategic goals, determining actions to achieve those goals, setting a timeline for execution, and allocating resources to execute the actions. Strategic planning can be long term, with action steps established from 2 to 5 years ahead. The senior leadership typically determines the strategy, which can be planned and intentional or observed as a pattern that emerges as part of planned activity.
Some key aspects of strategic planning include defining strategic goals, determining actions to achieve those goals, setting a timeline for execution, and allocating resources to execute the actions. Strategic planning can be long term, with action steps established from 2 to 5 years ahead. The senior leadership typically determines the strategy, which can be planned and intentional or observed as a pattern that emerges as part of planned activity.
Strategic planning in public health and health care has evolved over time, adapting and changing needs and contexts. In the 1960s, strategic planning gained prominence in the corporate world. It was seen as “the one best way” to enhance competitiveness by devising and implementing effective strategies (Mintzberg, 1994). According to Zuckerman (2016), health care organizations have used strategic planning sporadically since the 1970s. Back then, it was oriented toward meeting the needs of populations and providing health services (p. 5). In the 1990s, strategic planning faced criticism for being overly rigid and detached from reality. Planners shifted from creating strategies to providing data and helping managers think strategically. In the 2000s, public health strategic planning emphasized patient-/person-centered care; quality improvement; and adaptability to external factors like rapid technological advances, evolving patient needs, and regulatory changes.
Strategic planning continues to be crucial for anticipating challenges, allocating resources, and achieving organizational goals. In essence, strategic planning in public health and health care involves analyzing the agency’s various environments for strengths, weaknesses, opportunities, and threats; establishing a clear vision for the future of the organization and the communities it serves; and developing goals and effective strategies for sustainable growth and improved outcomes.
There are a myriad of models and frameworks designed to guide strategic planning in the public health and health care worlds. The frameworks listed below feature a few of these models most used in health care and often in public health as well. This is not a comprehensive look at all models or frameworks.
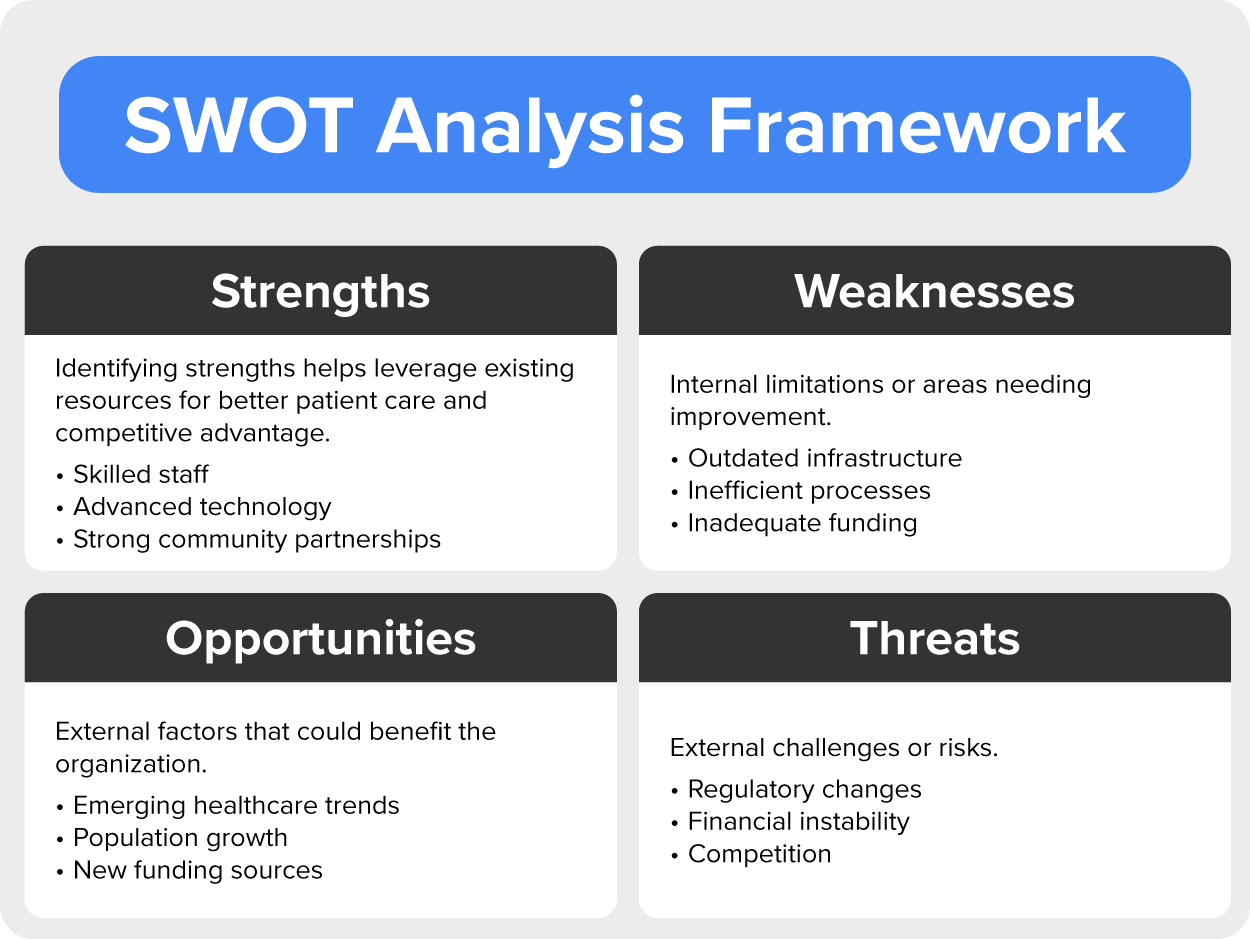
This framework tool is used to assess an organization’s internal strengths and weaknesses as well as the external opportunities and threats. The SWOT approach is a very common approach to strategic planning in health care and public health. Strengths are described as positive attributes within health care or public health organizations. Examples include skilled staff, advanced technology, or strong community partnerships. Identifying strengths helps leverage existing resources for better patient care and competitive advantage. Weaknesses are internal limitations or areas needing improvement. Examples might be outdated infrastructure, inefficient processes, or inadequate funding. Addressing weaknesses is essential for enhancing the overall performance.
Opportunities are external factors that could benefit the organization. Examples include emerging health care trends, population growth, or new funding sources. Capitalizing on opportunities allows for growth and innovation. Threats are external challenges or risks. Examples include regulatory changes, financial instability, or competition from other providers. Mitigating threats ensures organizational resilience. By analyzing these factors, health care leaders can make informed decisions, allocate resources effectively, and develop strategies that align with their mission and vision.
This framework helps organizations convert their mission and vision into specific, measurable goals across four perspectives: customer (patient satisfaction and outcomes), internal processes (efficiency, quality, and process improvement), financial (revenue and costs), and learning/growth (emphasizes staff development, innovation, and adaptability; Jackson, 2024).
This framework helps organizations proactively address external factors that could influence their strategic direction. Some external factors include political factors (tax policies that impact health care spending or subsidies by the government or employment law changes affecting staffing), economic factors (unemployment rates or interest rates directly or indirectly affecting financial performance), sociocultural factors (demographics, cultural shifts, and social trends, which all help in understanding patient preferences), and technological factors (advances in health care technology impacting service delivery, data management, and patient care). The extended version of PEST (PESTEL) adds environmental factors like environmental regulations, sustainability practices, and ecological impacts on health care operations and legal factors (compliance requirements and health care legislation; Siddiqui, 2021).
This framework focuses on navigating future uncertainties. It involves creating detailed narratives about different potential scenarios, helping health care organizations prepare for a range of possible developments. Examples of possible scenarios may include consumer behavior, health equity, and economic changes. Scenario planning involves monitoring signals and adjusting strategies as more information becomes available (agile; Riess & Bogus, 2020).
Frameworks provide a structured approach to strategic planning. They guide organizations through the process, ensuring that critical aspects are considered systematically. They also ensure consistency across different planning cycles and within the organization. Frameworks allow for standard terminology, processes, and evaluation criteria. Following these frameworks infuses strategic planning with best practices learned from successful organizations and can help organizations avoid common pitfalls and adopt proven strategies.
EXAMPLE
The image below depicts the Rhode Island Health Strategic Framework used by the State Department of Health (a public health organization). It shows a structured approach to guide the department. This is the result of substantial strategic planning by this health department. This framework is led by the three leading priorities (goals) the health department views as top public health issues for the state. This framework then depicts the five strategies proposed to be applied to meet the goals related to the three priorities.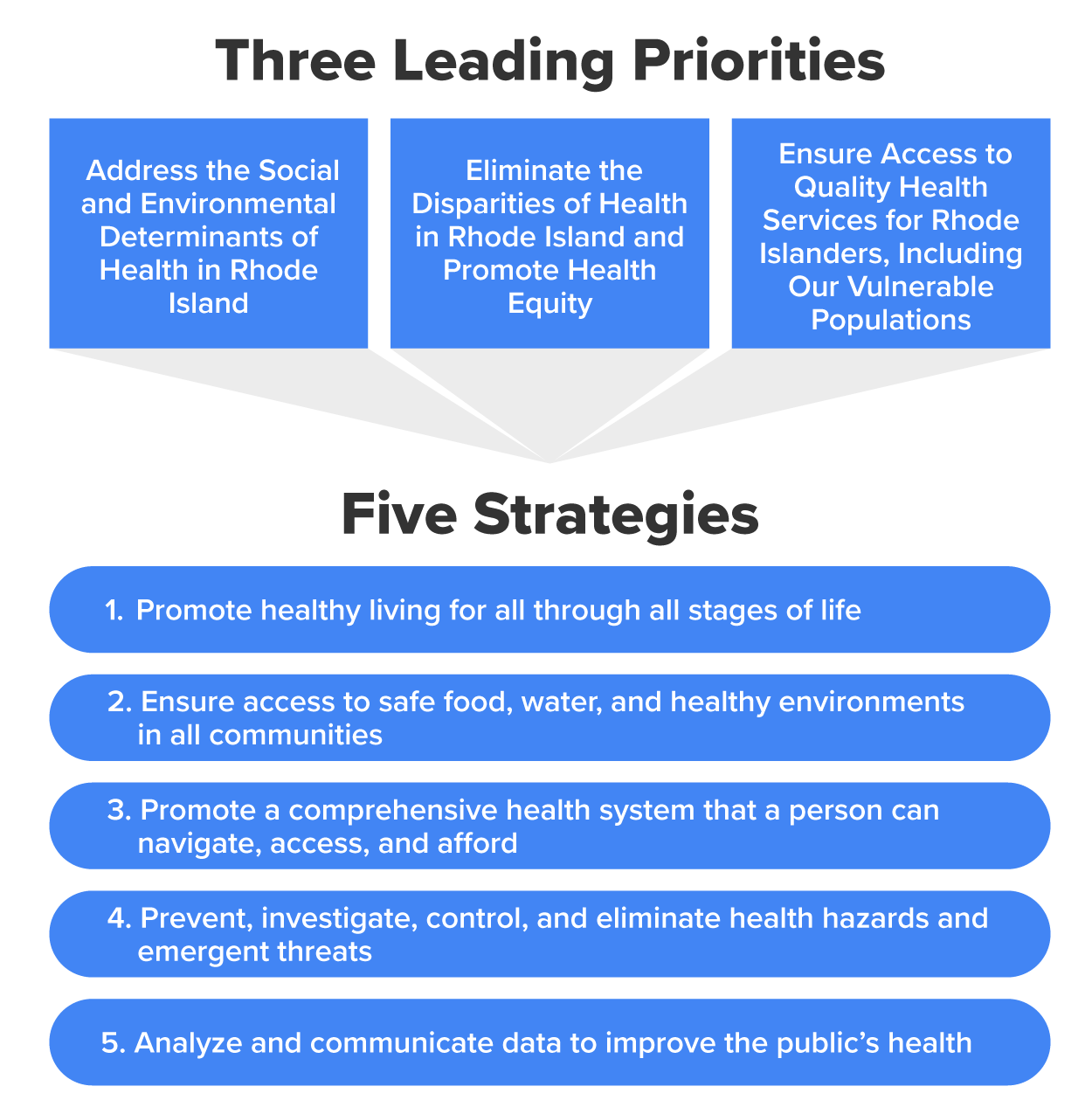
Rhode Island’s Strategic Framework aims to reduce health disparities and achieve health equity. There are 23 population health goals they are working toward. These include reducing obesity in children, teens, and adults; addressing chronic illnesses like diabetes and heart disease; promoting maternal and child health; enhancing senior health; focusing on behavioral health and wellness; supporting recovery and rehabilitation for substance use; improving access to healthy food that is affordable and safe; ensuring compliance with health standards related to clean water supplies; reducing environmental toxins like tobacco and lead; and ensuring safe and affordable housing, access to comprehensive health care, and many more. Rhode Island uses this strategic model to build capacity, to emphasize prevention needs assessment, and for effective program implementation and outcome evaluation.
Strategic planning models play a crucial role in shaping public and community health initiatives. While the frameworks discussed above focus on health care and public health organizations, there are two models that focus directly on community health. The table below describes the Mobilizing for Action Through Planning and Partnership (MAPP) model and the use of logic models.
| Model Name | Description |
|---|---|
| Logic models |
|
| MAPP |
|
The image below depicts a best practices logic model used in strategic planning. It is called the Behavior-Determinant-Intervention (BDI) logic model. As you can see by the illustration, the intended topic and target audience would be expectant mothers to address maternal and child health while pregnant.

Like other models, the BDI logic model helps in designing, implementing, and evaluating programs by ensuring that interventions directly influence specific determinants that affect core behaviors. In this case, the use of the model begins at the right (the pink box) by identifying the overall health goal and then specifying the targeted behavior (e.g., taking prenatal vitamins during pregnancy or a healthy diet during pregnancy) that need to be addressed to achieve the health goal. In the middle of the model below, determining the risk and protective factors means identifying what directly influences the targeted behavior(s). These could include social factors, knowledge, attitudes, and access to health care, for example. Finally, all the way to the left of the model, we design, implement, and evaluate plans for the intervention activities. Once the model is complete, the arrows reverse to represent whether the intervention activities directly and intentionally contributed to achieving the health goal. This and other logic models empower communities and health agencies to create targeted, effective interventions that improve overall health and well-being.
The image below depicts the MAPP model. This model is a community-driven strategic planning process designed to achieve health equity.
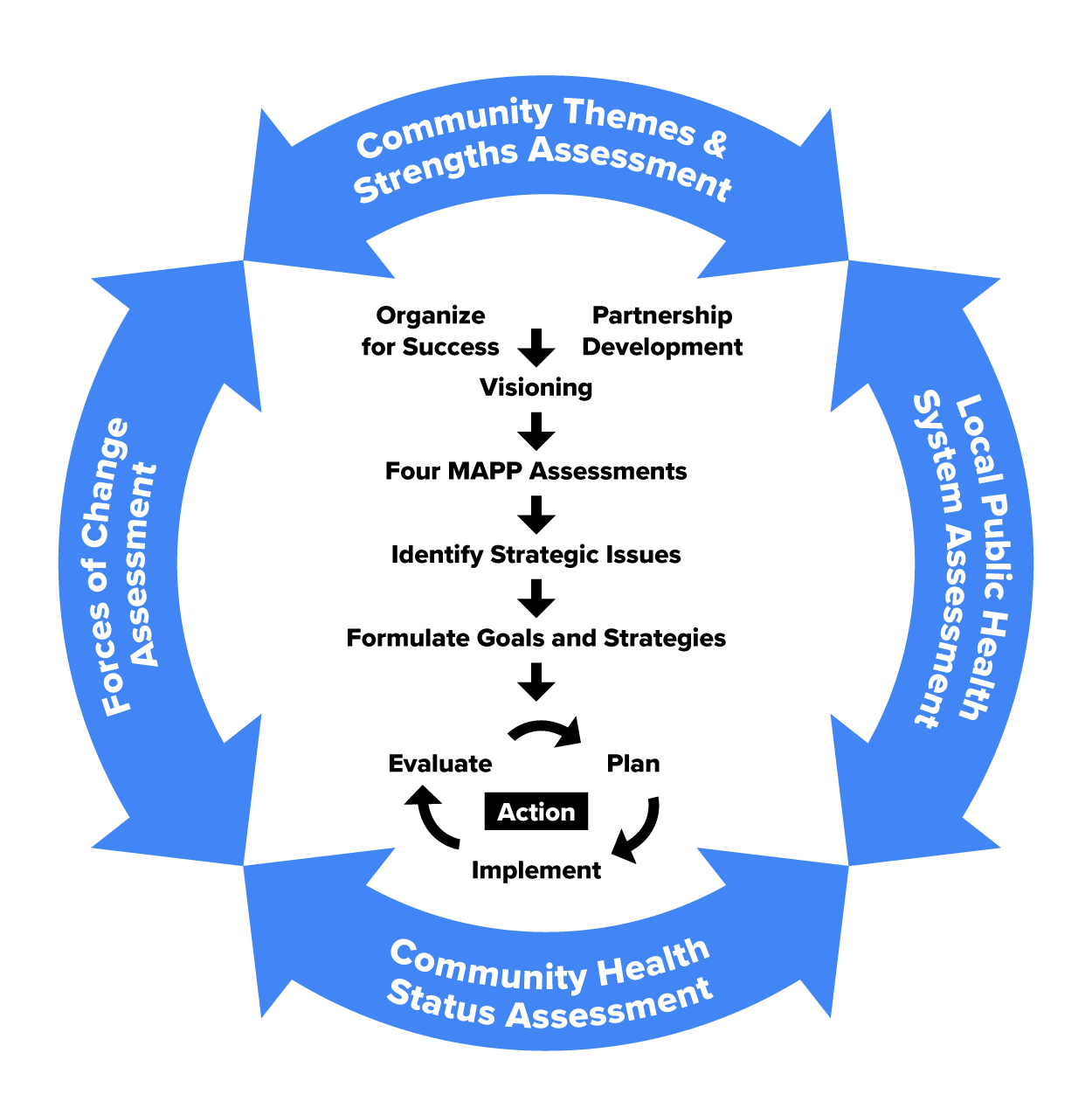
MAPP assesses the community’s most pressing population health issues and aligns resources across sectors for strategic action. Note that like other strategic planning processes, this begins with assessing priorities, getting the community and partners organized, setting the stage for a collaborative and creative process to develop a shared vision, and formulating strategies and goals.
Also in community health, strategic planning plays a crucial role in guiding local health departments (LHDs) and community health boards. A strategic plan provides a clear picture of where the organization (such as an LHD) is headed, what it aims to achieve, and how it plans to succeed. The plan defines the health department or community health board’s roles, priorities, and direction over 3 to 5 years. It specifies what the organization plans to achieve and outlines how those goals will be reached. It includes measures to monitor progress and assess success, and it guides decision-making, resource allocation, and the pursuit of objectives. It strengthens the organization’s ability to carry out its public health functions. LHDs seek national accreditation from the Public Health Accreditation Board (PHAB); to achieve it, a strategic plan is needed. Accreditation provides a structured approach to maintaining and advancing the quality and effectiveness of LHDs. Accreditation helps LHDs identify and implement performance improvement opportunities, ensuring they provide high-quality services to the community.
Strategic planning provides a clear picture of where an organization is headed. It outlines goals, objectives, and methods for achieving them, ensuring alignment with the organization’s mission and vision. With a solid plan, an organization can better justify funding levels and attract new funding. It helps allocate resources effectively to address critical public health needs. Strategic planning involves partnerships fostering collaboration and buy-in. It ensures community voices are heard and considered in the decision-making processes. A well-crafted plan allows organizations to adapt to changing environments, emerging health threats, and evolving community needs. Finally, having a strategic plan enables organizations to monitor progress, track outcomes, and be accountable to their communities and funders.
| Framework/Model Name | Description |
|---|---|
| SWOT | The framework tool is used to assess an organization’s internal strengths and weaknesses, as well as the external opportunities and threats. |
| BSC | This framework helps organizations convert their mission and vision into specific, measurable goals. |
| PEST/PESTEL analysis | This framework helps organizations proactively address external factors that could influence their strategic direction. The extended version of PEST (PESTEL) adds environmental factors like environmental regulations and sustainability practices and legal factors, which are laws, regulations, and legal constraints affecting operations |
| Scenario planning | This framework focuses on navigating future uncertainties. It involves creating detailed narratives about different potential scenarios, helping public health and health care organizations prepare for a range of possible developments. |
Source: THIS TUTORIAL WAS AUTHORED BY SOPHIA LEARNING. PLEASE SEE OUR TERMS OF USE.
Disclaimer: The use of any CDC and United States government materials, including any links to the materials on the CDC or government websites, does not imply endorsement by the CDC or the United States government of us, our company, product, facility, service, or enterprise.
REFERENCES
American Journal of Healthcare Strategy. (n.d.). Strategic planning for healthcare. ajhcs.org/strategic-planning-for-healthcare
Jackson, T. (2024, August 21). How to develop a balanced scorecard in healthcare - With examples. ClearPoint Strategy. www.clearpointstrategy.com/blog/the-balanced-scorecard-in-healthcare
Mintzberg, H. (1994). The fall and rise of strategic planning. Harvard Business Review. hbr.org/1994/01/the-fall-and-rise-of-strategic-planning
National Center for Chronic Disease Prevention and Health Promotion. (2015, March 12). Transforming communities to make healthy living easier. stacks.cdc.gov/view/cdc/32399
Riess, R., & Bogus, S. (2020, September). Health care strategy insights: Scenario planning. Deloitte. www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-scenario-planning-strategy-insights.pdf
Siddiqui, A. A. (2021). The use of PESTEL analysis tool of quality management in the health care business and its advantages. American Journal of Biomedical Science & Research, 14(6). dx.doi.org/10.34297/AJBSR.2021.14.002046
Zuckerman, A. (2016). Healthcare strategic planning (3rd ed.). Health Administration Press.