Table of Contents |
There are many reasons why it can be useful to control microbial growth. For example, someone may clean a dinner table before eating or clean a surface before preparing food on it. A doctor needs to reduce the risk of one patient spreading a pathogen to the next patient. Surgical instruments need to be especially clean, or infection after surgery would be common.
Control of microbial growth differs depending on the context. In this lesson, the focus is on microbes on surfaces. For example, one way to reduce the spread of disease is by cleaning the inanimate objects (fomites) on which microbes may be left by one person and picked up by another. In other lessons, you will learn about the ways in which medications are used to control pathogens inside the human body.
Two major considerations are especially important in choosing a method of microbial control on an object or surface. First, it is important to consider the way in which an object will be used. For example, a surgical instrument requires a much higher level of cleanliness than a kitchen table. For this purpose, items can be classified as critical (meaning that they must be sterile), semicritical (meaning that they require a high level of disinfection), or noncritical (meaning that they need to be clean but not highly disinfected).
EXAMPLE
Surgical instruments are critical items and must be sterile. A medical instrument that contacts intact skin but does not penetrate it (such as an endoscope used to view the esophagus) is semicritical. Bed linens and similar items are noncritical.Second, it is important to consider what potential pathogens are being targeted and how resistant they are to antimicrobial treatments. Some microbes, especially those that form endospores, require harsher treatments than more sensitive species.
In many clinical and laboratory settings, aseptic technique is used to prevent the contamination of sterile surfaces. Aseptic technique involves a combination of protocols to prevent microbial contamination. This approach is often used in the microbiology laboratory both to prevent contamination of the work area and to prevent the spreading of microbes from the work area.
In medical work, a sterile field is often designated and is kept free of all vegetative (actively growing) microbes, endospores, and viruses. For example, a sterile field is required around a surgical incision. Strict protocols are required to protect the sterility of the area, including the sterilization of equipment and materials. Introducing microbes into a patient’s body produces the risk of sepsis, a systemic inflammatory response to infection that is serious and can be lethal.
There are a variety of terms used to carefully describe the different types of microbial control. These terms are often used much more loosely in everyday conversation but have very specific meanings in microbiology. These terms are summarized below. In other lessons, you will learn more about the specific agents used for each.
The following terms refer to treatments used on inanimate surfaces or items.
| Common Protocols for Control of Microbial Growth | |||
|---|---|---|---|
| Protocol | Definition | Common Application | Common Agents |
| For Use on Fomites | |||
| Sterilization | Completely eliminates all vegetative cells, endospores, and viruses from an inanimate item | Preparation of surgical equipment and needles used for injections | Pressurized steam (autoclave), chemicals, and radiation |
| Disinfection | Reduces or destroys the microbial load of an inanimate item through the application of heat or antimicrobial chemicals | Cleaning surfaces like laboratory benches, clinical surfaces, and bathrooms | Chlorine bleach, phenols (e.g., Lysol), and glutaraldehyde |
| Sanitization | Reduces the microbial load of an inanimate item to safe public health levels through the application of heat or antimicrobial chemicals | Commercial dishwashing of eating utensils and cleaning of public restrooms | Detergents containing phosphates (e.g., Finish) and industrial-strength cleaners containing quaternary ammonium compounds |
| For Use on Living Tissue | |||
| Antisepsis | Reduces the microbial load on skin or tissue through the application of an antimicrobial chemical | Cleaning skin that is broken because of injury or before surgery | Boric acid, isopropyl alcohol, hydrogen peroxide, and iodine (betadine) |
| Degerming | Reduces the microbial load on skin or tissue through gentle to firm scrubbing and the use of mild chemicals | Handwashing | Soap and alcohol swabs |
There is terminology to describe the extent to which different physical and chemical methods affect microbes. The suffix -cide (or -cidal) indicates that something kills, whereas the suffix -stat (or -static) indicates that something inhibits growth. For example, a virucide kills viruses and a fungicide kills fungi. In contrast, a bacteriostatic chemical inhibits growth without killing the bacteria already present. Whether a particular treatment is -cidal or -static is determined by the types of microorganisms targeted, the concentration of the chemical used, and the type of treatment applied (e.g., the type of chemical or physical method used).
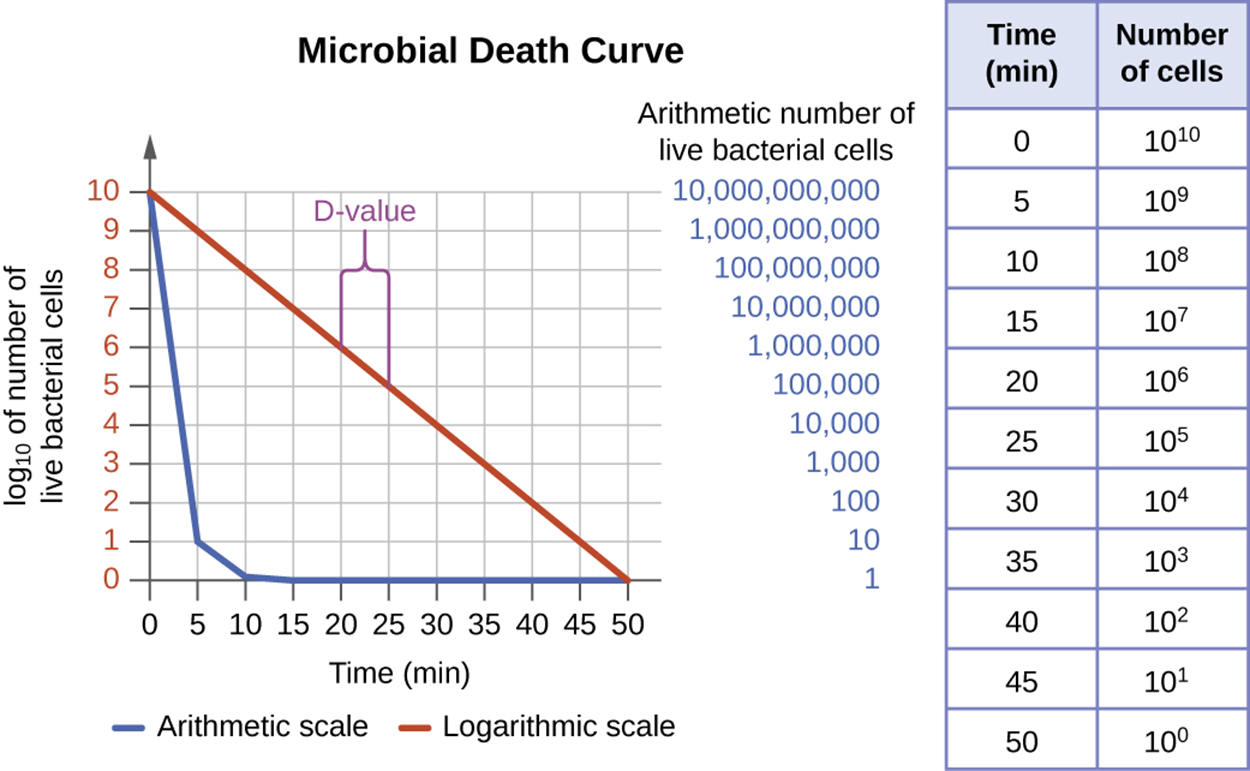
The image below shows a microbial death curve, which is used to describe the progress and effectiveness of a particular protocol. Over time, exposure to a protocol will lead to a fixed percentage of microbes in a population dying per unit of time. The rate of death is constant regardless of the initial population size, so it is often valuable to know the percentage of the population that has been killed. As shown in the image below, this can be useful to plot death curves as semilog plots because the reduction in microorganisms is typically logarithmic. The D-value labeled on the image is the decimal reduction time (DRT), which is the amount of time it takes for a specific protocol to kill 90% of the population.
Source: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “MICROBIOLOGY.” ACCESS FOR FREE AT openstax.org/details/books/microbiology. LICENSE: CC ATTRIBUTION 4.0 INTERNATIONAL.