Table of Contents |
Abbreviations:
GFR - glomerular filtration rate
RPF - renal plasma flow
PGC - glomerular pressure
PAA - afferent arteriole pressure
PEA - efferent arteriole pressure
RAA - afferent arteriole resistance
REA - efferent arteriole resistance
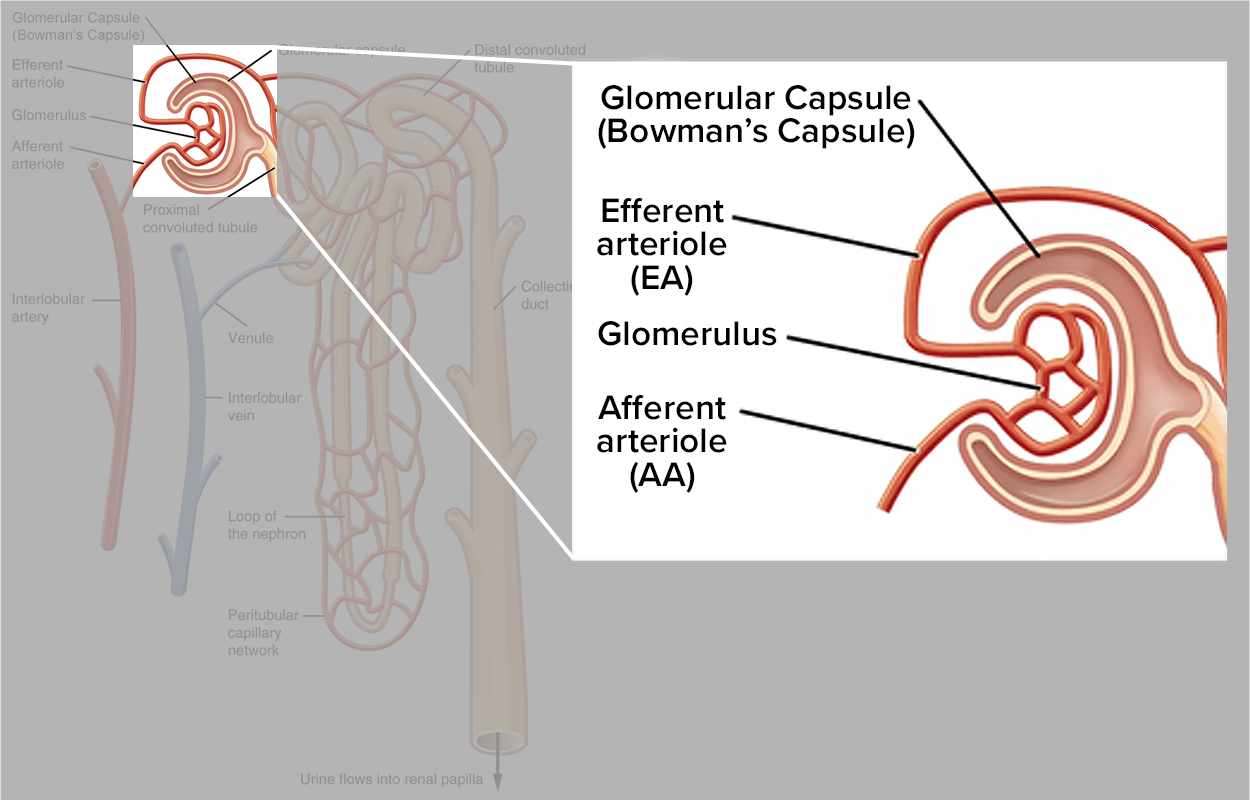
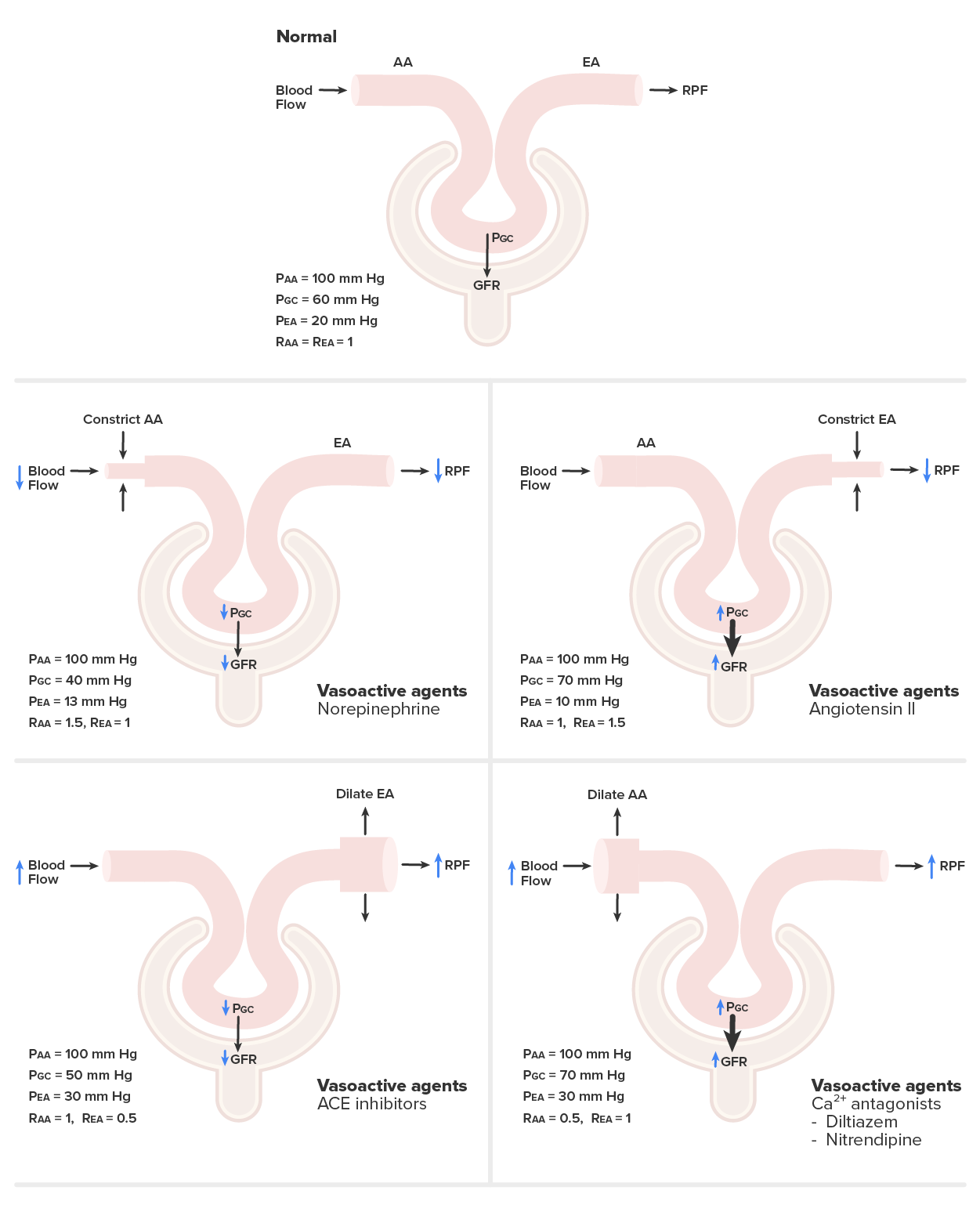
The kidney’s afferent and efferent arterioles are unique in that they are two resistance vessels in series. Therefore, there can be different effects when one is constricted or dilated and the other is not, as shown above (this usually happens with certain drugs). For example:
The kidneys are very effective at regulating the rate of blood flow over a wide range of blood pressures. Your blood pressure will decrease when you are relaxed or sleeping. It will increase when exercising. Yet, despite these changes, the filtration rate through the kidney will change very little. This is due to two internal autoregulatory mechanisms that operate without outside influence: the myogenic mechanism and the tubuloglomerular feedback mechanism.
The myogenic mechanism regulating blood flow within the kidney depends upon a characteristic shared by most smooth muscle cells of the body. When you stretch a smooth muscle cell, it contracts; when you stop, it relaxes, restoring its resting length. This mechanism works in the afferent arteriole that supplies the glomerulus. When blood pressure increases, smooth muscle cells in the wall of the arteriole are stretched and respond by contracting to resist the pressure, resulting in little change in flow. When blood pressure drops, the same smooth muscle cells relax to lower resistance, allowing a continued even flow of blood.
The tubuloglomerular feedback mechanism involves the JGA and a paracrine signaling mechanism utilizing ATP, adenosine, and nitric oxide (NO). This mechanism stimulates either contraction or relaxation of afferent arteriolar smooth muscle cells. Recall that the DCT is in intimate contact with the afferent and efferent arterioles of the glomerulus. Specialized macula densa cells in this segment of the tubule respond to changes in the fluid flow rate and Na⁺ concentration.
As GFR increases, there is less time for NaCl to be reabsorbed in the PCT, resulting in higher osmolarity in the filtrate. The increased fluid movement more strongly deflects single nonmotile cilia on macula densa cells. This increased osmolarity of the forming urine, and the greater flow rate within the DCT, activates macula densa cells to respond by releasing ATP and adenosine (a metabolite of ATP).
ATP and adenosine act locally as paracrine factors to stimulate the myogenic juxtaglomerular cells of the afferent arteriole to constrict, slowing blood flow and reducing GFR. Conversely, when GFR decreases, less Na⁺ is in the forming urine, and most will be reabsorbed before reaching the macula densa, which will result in decreased ATP and adenosine, allowing the afferent arteriole to dilate and increase GFR. NO has the opposite effect, relaxing the afferent arteriole at the same time ATP and adenosine are stimulating it to contract. Thus, NO fine-tunes the effects of adenosine and ATP on GFR.
| Change in GFR | NaCl Absorption | Role of ATP and adenosine/Role of NO | Effect on GFR |
|---|---|---|---|
| Increased GFR | Tubular NaCl increases | ATP and adenosine increase, causing vasoconstriction | Vasoconstriction slows GFR |
| Decreased GFR | Tubular NaCl decreases | ATP and adenosine decrease, causing vasodilation | Vasodilation increases GFR |
| Increased GFR | Tubular NaCl increases | NO increases, causing vasodilation | Vasodilation increases GFR |
| Decreased GFR | Tubular NaCl decreases | NO decreases, causing vasoconstriction | Vasoconstriction decreases GFR |
| Term | Pronunciation | Audio File |
|---|---|---|
| Myogenic | myo·gen·ic |
|
| Tubuloglomerular | tu·bu·lo·glo·mer·u·lar |
|
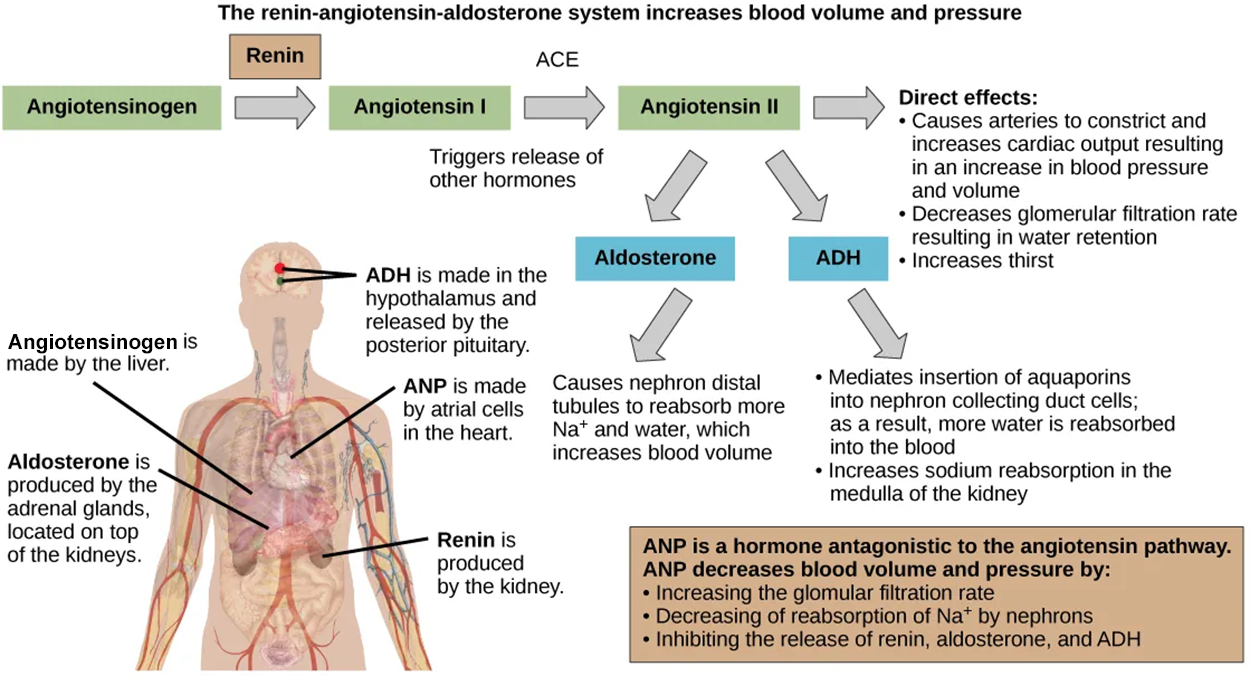
The renin–angiotensin–aldosterone system (RAAS), illustrated below, critically regulates blood pressure and blood volume over the long term. This system proceeds through several steps to produce angiotensin II, acting to stabilize blood pressure and volume. Renin (secreted by a part of the juxtaglomerular complex) is produced by the granular cells of the afferent and efferent arterioles. Thus, the kidneys directly control blood pressure and volume.
Renin acts on angiotensinogen, which is made in the liver, and converts it to angiotensin I. Angiotensin converting enzyme (ACE) converts angiotensin I to angiotensin II. Angiotensin II raises blood pressure by constricting blood vessels. It also triggers the release of the mineralocorticoid aldosterone from the adrenal cortex, which in turn stimulates the renal tubules to reabsorb more sodium. Angiotensin II also triggers the release of antidiuretic hormone (ADH) from the hypothalamus. You may recall from a previous lesson that ADH promotes water retention in the kidneys by signaling the kidneys to reabsorb water. It acts directly on the nephrons and decreases the glomerular filtration rate.
Specialized cells in the wall of the atria produce and secrete the peptide hormone atrial natriuretic peptide (ANP). ANP signals the kidneys to reduce sodium reabsorption, thereby decreasing the amount of water reabsorbed from the urine filtrate and reducing blood volume. Other actions of ANP include the inhibition of renin secretion, which inhibits the RAAS and promotes vasodilation, and ADH secretion, which also affects kidney function. Therefore, ANP aids in decreasing blood pressure, blood volume, and blood sodium levels
| Term | Pronunciation | Audio File |
|---|---|---|
| Renin–Angiotensin–Aldosterone | re·nin an·gio·ten·sin al·do·ste·rone |
|
| Antidiuretic | an·ti·di·uret·ic |
|
Source: THIS TUTORIAL HAS BEEN ADAPTED FROM (1) "ANATOMY AND PHYSIOLOGY 2E" ACCESS FOR FREE AT OPENSTAX.ORG/DETAILS/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E. (2) "BIOLOGY FOR AP COURSES" ACCESS FOR FREE AT OPENSTAX.ORG/DETAILS/BOOKS/BIOLOGY-AP-COURSES. LICENSING (1 & 2): CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL