Table of Contents |
There is a wide variety of ways in which microbial growth can be influenced by physical means. Some approaches cause damage to cell structures or metabolic functions, whereas others remove microbes from substances. There are reasons why certain methods are more useful than others in particular circumstances. Additionally, the types of equipment needed and ease of use varies. In this lesson, you will learn about an assortment of physical methods to control microbial growth and how these methods are commonly used.
One of the most commonly used and oldest approaches to controlling microbial growth is using heat. This is a part of the daily life of most people.
EXAMPLE
Cooking food can kill foodborne pathogens. You may have experienced a “boil water order” due to contamination of the water supply, meaning that you needed to boil water to remove vegetative cells that might otherwise cause disease. Boiling is generally not sufficient to eliminate endospores except over very extended periods (20 hr) or with a very specific protocol of repeated boiling, cooling to allow time to germinate, and boiling again (tyndallization; Piqué et al., 2019).The reason why heat is effective as a control method is that it denatures proteins and disrupts cell membranes. Although some hyperthermophiles are remarkably resistant to heat, there are temperatures beyond which no cells are known to survive.
Different microbes are susceptible to different levels of heating, and there are several ways to describe this. The thermal death point (TDP) of a microorganism is the lowest temperature at which all microbes are killed in 10 min of exposure. The thermal death time (TDT) is the length of time needed to kill all microorganisms in a sample at a given temperature.
Heat can be used for sterilization through two major categories of protocols: moist-heat sterilization and dry-heat sterilization. Dry-heat sterilization is frequently used in the laboratory, as shown in the image below. Image (a) shows an inoculating loop used to transfer bacteria from one location to another. This loop is being held over a Bunsen burner to heat it. Image (b) shows a newer, safer method of accomplishing the same thing. An inoculating loop can be inserted into the cylindrical chamber to be heated.
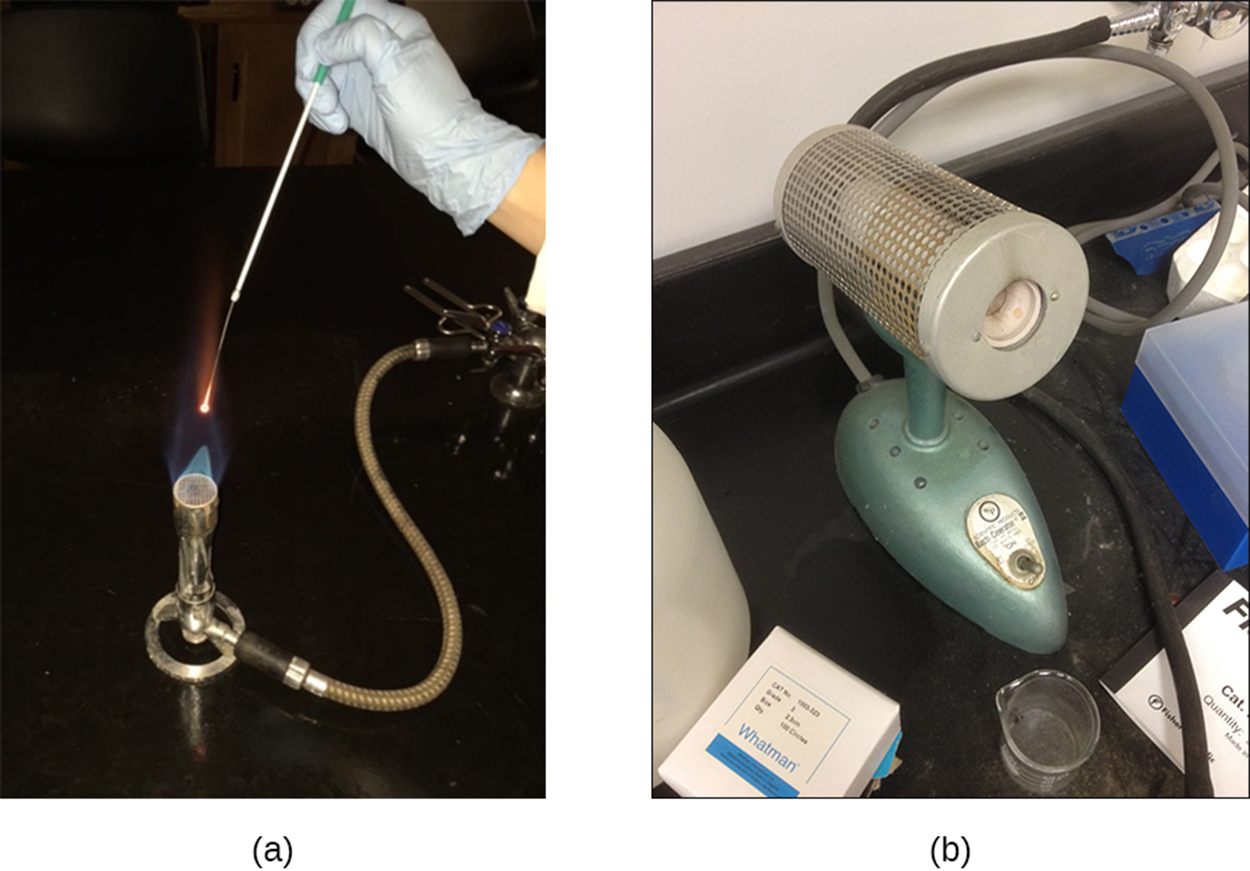
Dry-heat sterilization has some advantages. For example, powders can be sterilized in this manner. Using a dry-heat sterilizer, such as an oven, substances can be heated for at least 2 hr at temperatures of up to 170 °C. However, dry-heat sterilization is slower and generally less effective than moist-heat sterilization, which penetrates cells more effectively.
The image below shows an autoclave, which is an extremely common method of carrying out moist-heat sterilization and is generally considered the most effective method for materials that can withstand the heat. Materials to be sterilized are placed in the chamber and heated in a moist environment at high pressure. The first autoclave was developed by Charles Chamberland (1851–1908).

Autoclaves generally work by removing air from the chamber and replacing it with steam, resulting in increased interior pressure and temperatures above the boiling point of water. In gravity displacement autoclaves, steam is introduced from the top or sides of the chamber and the heavier air in the chamber sinks to the bottom to be forced out through a vent. In prevacuum sterilizers, a high-speed vacuum is used to completely remove air before steam is introduced into the chamber. This type of sterilizer allows steam to more effectively penetrate wrapped items because air is more completely removed.
Many modern autoclaves can work in either way. Gravity displacement cycles are used for the decontamination of waste and sterilization of unwrapped glassware, whereas prevacuum sterilization is used for the sterilization of packaged instruments.
In large industrial settings, especially large autoclaves called retorts are used to allow very large-scale sterilization of materials.
The standard operating temperatures for autoclaves are 121 °C or sometimes 132 °C at pressures of 15–20 psi. Although the length of time required depends on the material to be sterilized, cycles are generally 20 min or more, with longer times required for larger volumes of materials. The steam must contact the materials to be sterilized, so containers are left loosely closed and instruments are loosely wrapped.
To ensure that the conditions in the autoclave reach those necessary for sterilization, indicators are often used. The image below shows two test tubes of growth medium. Each tube is wrapped with a piece of tape. The tube on the left has plain tape, indicating that it has not been sterilized. The tube on the right has a diagonal black line that appears once the conditions for sterilization have been met and indicates that it has been sterilized.
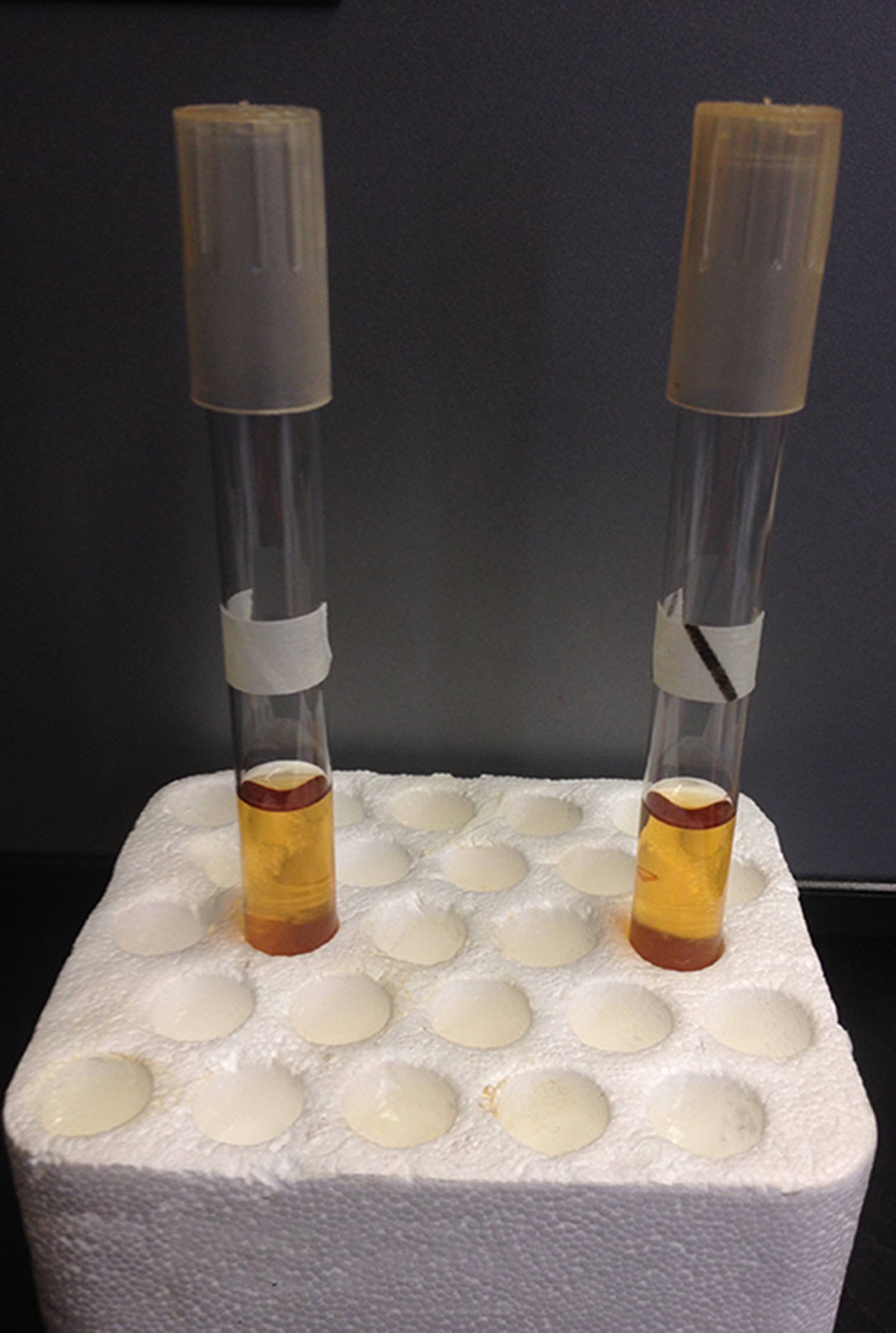
Although indicator tape of this type is convenient, it is not sufficient for the most critical sterilization procedures. For example, this type of tape does not indicate how long the high temperature conditions were maintained. Another type of indicator, a biological indicator spore test, uses a strip of paper or a liquid suspension of endospores of Geobacillus stearothermophilus to determine whether the endospores are killed or able to grow. These spores are unusually heat resistant. If they are able to germinate after autoclaving, then the sterilization procedure was not adequate.
Finally, Diack tubes can also be used as indicators for autoclaves. These are glass ampules that each contain a temperature-sensitive pellet that melts at the proper sterilization temperature.
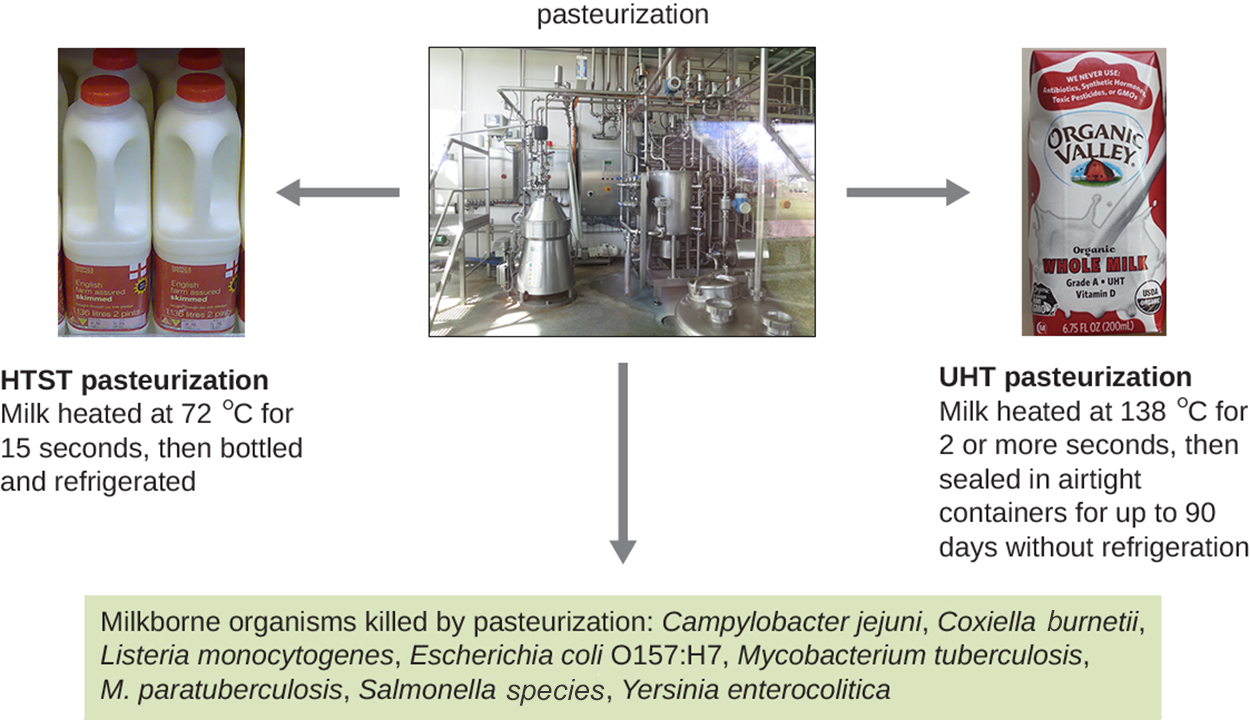
Another microbial control method using heat is pasteurization, which reduces food spoilage but does not sterilize. Pasteurization involves heating food or liquids (such as milk) sufficiently to kill pathogens and spoilage-causing microbes, but it does not kill spores.
Traditional pasteurization, developed by Louis Pasteur in the 1860s, was used to help preserve beer and wine. Pasteur used temperatures around 57 °C and temperatures of approximately 63 °C have been used, but this requires maintaining a high temperature for approximately 30 min (Britannica, 2022). More recently, newer approaches have been developed and are commonly used for milk and orange juice, among other products. High-temperature short-time (HTST) pasteurization exposes milk to a temperature of 72 °C for 15 s.
Ultra-high-temperature (UHT) pasteurization exposes milk to a temperature of 138 °C for 2 s or more. UHT milk can be stored in sealed containers without refrigeration for extended times without spoilage.
The image below summarizes the types of pasteurization, including traditional, HTST, and UHT pasteurization, and gives examples of milkborne pathogens that are killed by these approaches (Campylobacter jejuni, Coxiella burnetii, Listeria monocytogenes, the pathogenic Escherichia coli strain O157:H7, Mycobacterium tuberculosis, M. paratuberculosis, Salmonella species, and Yersinia entercolitica).
Other common methods of controlling microbial growth are refrigeration and freezing. Many people use these approaches daily with home refrigerators and freezers.
Home and laboratory refrigerators generally maintain temperatures between 0 °C and 7 °C, which is sufficient to slow microbial growth and slow food spoilage. When the temperature is lowered to −2 °C or below, then susceptible organisms may be killed.
Because some organisms may be dormant at low temperatures, it is important to thaw food carefully. The U.S. Department of Agriculture (USDA) has guidelines regarding the appropriate ways to handle food to reduce the risk of foodborne illness. Among these guidelines, the USDA includes recommendations to thaw food in the refrigerator, immerse it in cold water that is changed every 30 min, or thaw it using a microwave.
It is sometimes necessary to store specimens at low temperatures for extended periods of time. Special ultra-low freezers are available for laboratory use. Dry ice or liquid nitrogen tanks can also be used to maintain very low temperatures.
High pressure can also be used to kill microbes. High-pressure processing (pascalization) is used to kill bacteria, yeast, molds, parasites, and viruses in foods. This requires pressures between 100 and 800 MPa (compared with 0.1 MPa at sea level), but endospores can survive this treatment.
Another way that pressure is used is through hyperbaric oxygen therapy. A special chamber called a hyperbaric chamber provides an environment in which a patient is exposed to pure oxygen at pressures higher than the atmospheric pressure (typically between 1 and 3 atmospheres [atm], compared with the standard atmospheric pressure of 1 atm at sea level). The increased oxygen concentration can enhance the immune response and inhibit the growth of certain pathogens, although there are also risks such as oxygen toxicity and damage to delicate tissues from the pressure.
Although autoclaves use high pressure, the high temperature and moist heat rather than the pressure is responsible for killing pathogens.
Drying (desiccation) is another old method of preserving food. Like all living organisms, microbes need water for metabolism and survival. When food is dried out, it lasts longer without spoilage because microbes are unable to grow on it.
Foods can be dried naturally in the sun or freeze-dried (lyophilization). In freeze-drying, an item is rapidly frozen and placed under a vacuum so that water is lost by sublimation. This means that both cold temperatures and desiccation inhibit growth. Lyophilization causes less damage to the food item than conventional desiccation, and foods preserved this way can be stored without refrigeration if packaged appropriately so that they stay dry.
It is possible to lower the availability of water to microbes without physical drying by adding solutes such as salts and sugars. When a food item has a high concentration of salt or sugar, water is drawn out of cells by osmosis. That is why candied and salted foods were very important for food preservation before the development of refrigerators.
The image below shows an illustration of water leaving a cell through osmosis in a solute-rich environment in part (a). Part (b) shows examples of foods preserved through drying (raisins and jerky), salting (fish), and the addition of sugar (jam).

Exposure to various types of radiation can kill or inhibit microbes by damaging cellular structures and potentially causing mutations. Ionizing radiation (such as x-rays, gamma rays, and high-energy electron beams) can penetrate into cells and damage internal structures. In particular, double-stranded DNA may break and mutations may occur.
Because x-rays and gamma rays penetrate plastic and paper, they can be used to sterilize materials that cannot withstand the heat of an autoclave. This is how many materials such as plastic petri dishes, gloves, tubing, and plastic inoculating loops are sterilized. Gamma irradiation is also used on food in some countries. People who work with this type of radiation must protect themselves and their clothing, or barriers of iron or lead are used as they block even this highly penetrating radiation.
Nonionizing radiation such as ultraviolet light is often used for disinfection but does not use as much energy or penetrate as deeply as ionizing radiation. It can cause mutations that lead to cell death. It is commonly used in germicidal lights and water purification systems.
Another way to damage cell structures is through sonication, which means using high-frequency ultrasound waves. These waves cause changes in pressure in intracellular liquid that cause bubble formation within the cell. Structures within the cell become damaged, and the cell can eventually burst or collapse.
In the laboratory, sonication is used to lyse cells for research purposes and to clean equipment such as surgical instruments.
Filtration does not kill microbes, but it separates microbes from samples or environments. This can even sterilize a sample if the material being used as a filter has fine enough pores to catch all microbes.
A very common type of filtration is high-efficiency particulate air (HEPA) filtration. HEPA filters are used in air purifiers found in homes and offices. They are also found in vacuum cleaners. Biological safety cabinets use HEPA filters to prevent microbes from entering, exiting, or both. Hospitals often use HEPA filters to help prevent pathogens from spreading through ventilation systems or through the air in surgical suites. Areas of particular concern, such as isolation and burn units, may require special HEPA filters to keep the air quality very high.
The image below shows a photo of a square HEPA filter in part (a) and an illustration of a HEPA filter in part (b). In part (b), it is possible to see that there are sheets of filter medium inside a frame, and that particles such as microbes become trapped in the randomly arranged fibers of the filter sheet.
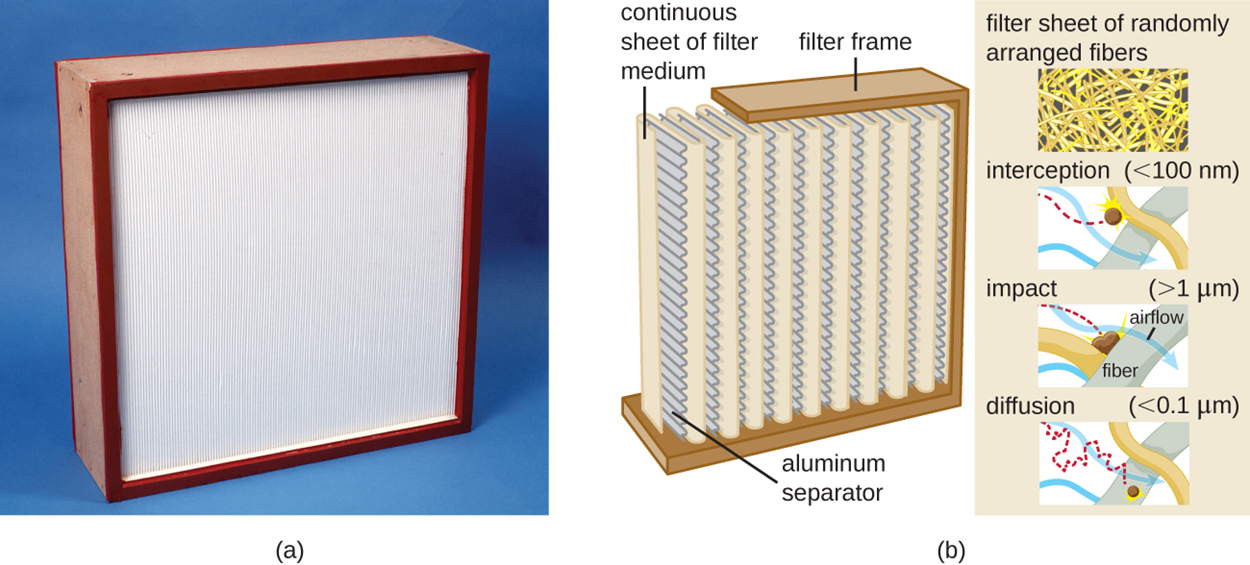
Membrane filters are used to remove microbes from liquids. They generally have an effective pore size of 0.2 μM, although smaller sizes are available. These can be very helpful when bacteria need to be removed from a heat-sensitive solution.
The table below summarizes all of the physical methods of control described in this chapter, including the conditions required, modes of action, and example uses.
| Physical Methods of Control | |||
|---|---|---|---|
| Method | Conditions | Modes of Action | Example Uses |
| Heat | |||
| Boiling | 100 °C at sea level | Denatures proteins and alters membranes | Cooking, personal use, and preparing certain laboratory media |
| Dry-heat oven | 170 °C for 2 hr | Denatures proteins and alters membranes, causes dehydration, and causes desiccation | Sterilization of heat-stable medical and laboratory equipment and glassware |
| Incineration | Exposure to flame | Destroys by burning | Flaming loop and microincinerator |
| Autoclave | Typical settings: 121 °C for 15 min at 15 psi | Denatures proteins and alters membranes | Sterilization of microbiological media, heat-stable medical and laboratory equipment, and other heat-stable items |
| Pasteurization | Can vary; one type is 72 °C for 15 s (HTST) | Denatures proteins and alters membranes | Prevents spoilage of milk, apple juice, honey, and other ingestible liquids |
| Cold | |||
| Refrigeration | 0 °C to 7 °C | Inhibits metabolism (slows or arrests cell division) | Preservation of food or laboratory materials (solutions and cultures) |
| Freezing | Below −2 °C | Stops metabolism and may kill microbes | Long-term storage of food, laboratory cultures, or medical specimens |
| Pressure | |||
| High-pressure processing | 100–800 MPa | Denatures proteins and can cause cell lysis | Preservation of food |
| Hyperbaric oxygen therapy | Oxygen air pressure three times higher than normal | Inhibits metabolism and the growth of anaerobic microbes | Treatment of certain infections (e.g., gas gangrene) |
| Desiccation | |||
| Simple desiccation | Drying | Inhibits metabolism | Dried fruits or jerky |
| Reduced water activity | Addition of salt or water | Inhibits metabolism and can cause lysis | Salted meats and fish, honey, jams, and jellies |
| Lyophilization | Rapid freezing under vacuum | Inhibits metabolism | Preservation of food, laboratory cultures, or reagents |
| Radiation | |||
| Ionizing radiation | Exposure to x-rays or gamma rays | Alters molecular structures and introduces double-strand breaks into DNA | Sterilization of spices and heat-sensitive laboratory and medical items; used for food sterilization in Europe but not widely accepted in the United States |
| Nonionizing radiation | Exposure to ultraviolet light | Introduces thymine dimers, leading to mutations | Disinfection of surfaces in laboratories and rooms in health care environments and disinfection of water and air |
| Sonication | |||
| Sonication | Exposure to ultrasonic waves | Cavitation (formation of empty space) disrupts cells, lysing them | Laboratory research to lyse cells; cleaning jewelry, lenses, and equipment |
| Filtration | |||
| HEPA filtration | Use of HEPA filter with 0.3-μm pore size | Physically removes microbes from air | Laboratory biological safety cabinets, operating rooms, isolation units, heating and air conditioning systems, and vacuum cleaners |
| Membrane filtration | Use of membrane filter with 0.2-μm or smaller pore size | Physically removes microbes from liquid solutions | Removal of bacteria from heat-sensitive solutions like vitamins, antibiotics, and media with heat-sensitive components |
Source: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “MICROBIOLOGY.” ACCESS FOR FREE AT openstax.org/details/books/microbiology. LICENSE: CC ATTRIBUTION 4.0 INTERNATIONAL.
REFERENCES
Britannica, T. Editors of Encyclopaedia (2022, September 6). pasteurization. Encyclopedia Britannica. www.britannica.com/technology/pasteurization
Piqué, N., Berlanga, M., & Miñana-Galbis, D. (2019). Health benefits of heat-killed (Tyndallized) probiotics: An overview. International journal of molecular sciences, 20(10), 2534. doi.org/10.3390/ijms20102534