Table of Contents |
Managing costs and revenue in healthcare organizations is a complex process that is essential for ensuring financial sustainability and the efficient delivery of care. Healthcare organizations, ranging from hospitals and medical centers to private practices and long-term care facilities, operate in an environment characterized by high operational costs, fluctuating patient volumes, regulatory compliance demands, and shifting reimbursement standards.
One of the primary tasks involved in cost management is controlling operational expenses, which consist of the bulk of a healthcare organization’s expenditures. These costs can mainly be categorized into fixed and variable costs. Fixed costs are those that remain constant regardless of the level of services provided, such as salaries of permanent staff, rent, and equipment depreciation. Variable costs, on the other hand, fluctuate with the volume of services provided, including supplies, medications, and hourly labor. Effective cost management requires healthcare administrators to carefully monitor and optimize both categories.
EXAMPLE
While fixed costs may be less flexible, organizations can often adjust variable costs through careful resource allocation and strategies that can save money. The use of supply chain management software, bulk purchasing agreements, and renegotiating vendor contracts can help reduce costs without sacrificing quality.Another significant aspect of cost management in healthcare is staffing. Labor is one of the largest expenses for any healthcare organization, including not just salaries but also benefits, training, and recruitment. Optimizing staffing levels through strategies such as workforce planning, job design, and productivity improvements is crucial. Understaffing can lead to increased patient complications, longer recovery times, and higher rates of readmission, all of which can drive up costs. On the other hand, overstaffing can result in inefficiency and unnecessary expenses. The use of data analytics to predict patient volumes, identify trends, and allocate resources effectively is becoming increasingly important in healthcare finance.
Revenue management in healthcare is equally challenging due to the often-unpredictable nature of reimbursements and the complexity of billing. Healthcare organizations typically receive revenue from multiple sources, including private insurance, government programs like Medicare and Medicaid, and out-of-pocket payments from patients. Each payer has its own reimbursement policies, which may vary by service, diagnosis, or procedure. Healthcare administrators must ensure that billing is accurate and timely to optimize reimbursements. This requires a strong understanding of coding systems such as ICD-10 (International Classification of Diseases) and CPT (Current Procedural Terminology), as well as knowledge of payer-specific rules and regulations.
Managing patient collections is another critical component of revenue management. While third-party payers like insurance companies contribute a substantial portion of healthcare revenue, patients themselves are increasingly responsible for higher out-of-pocket costs due to higher deductibles and co-pays. This has led to an increase in patient balances, making collections a crucial task for healthcare organizations. Effective revenue cycle management (RCM) includes pre-service, point-of-service, and post-service collection strategies. This involves verifying insurance coverage before services are rendered, collecting co-pays and deductibles upfront, and implementing effective billing and follow-up procedures for outstanding balances. Healthcare organizations can improve collections by offering payment plans, using technology for billing reminders and payments, and ensuring that staff are well-trained in customer service and payment negotiation.
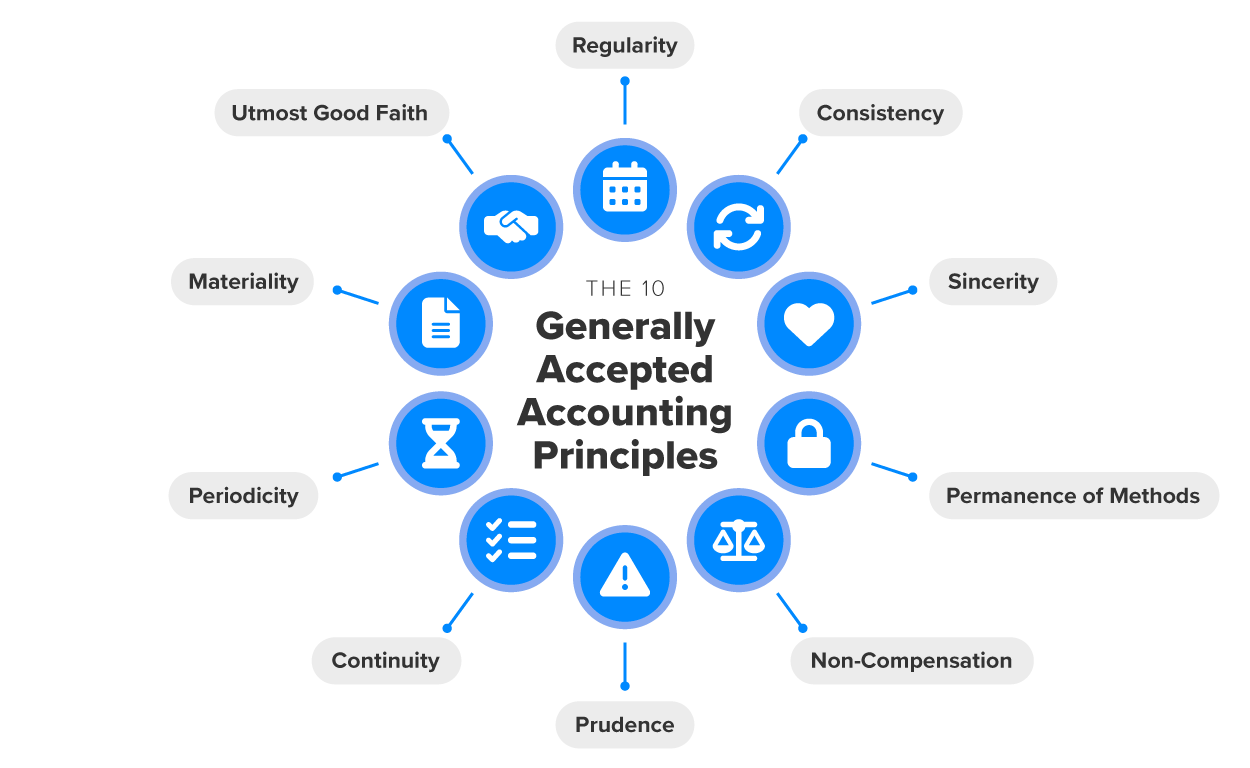
In addition to these direct cost and revenue management tasks, healthcare organizations must also comply with regulatory compliance and reporting requirements. Governments and accrediting bodies impose strict standards on how healthcare organizations must manage their finances, including maintaining transparency, conducting audits, and ensuring appropriate use of funds. The Affordable Care Act (ACA), for example, introduced new financial reporting requirements for healthcare organizations, including value-based purchasing programs and quality performance measures. Financial reporting must adhere to Generally Accepted Accounting Principles (GAAP), a set of standardized accounting rules and guidelines used in the United States to ensure consistency, transparency, and accuracy in financial reporting across organizations. Many organizations must also comply with specific rules for nonprofit entities if they are exempt from certain taxes. Failure to comply with these regulations can result in penalties, fines, and loss of accreditation, all of which can severely impact the financial health of the organization.
Technology plays a critical role in both cost and revenue management in healthcare. Advanced financial management software can help healthcare administrators track and manage revenue cycles, identify inefficiencies, and forecast financial performance. Additionally, the use of electronic health record (EHR) systems allows for better coding accuracy and improves billing practices, reducing errors that could result in delayed or denied reimbursements. Data analytics tools can also be used to track performance metrics, identify trends, and make more informed financial decisions. As healthcare becomes more data-driven, organizations are increasingly adopting artificial intelligence and machine learning algorithms to optimize cost control and revenue generation.
Financial governance in healthcare is the framework of policies, procedures, and practices that ensure the responsible management of financial resources within healthcare organizations. It plays a critical role in maintaining financial stability, ensuring compliance with regulations, and guiding the organization toward its long-term goals. This governance encompasses not only managing costs and revenues but also overseeing financial planning, risk management, internal controls, and transparency in reporting. Given the complexity of healthcare delivery, financial governance must address both the operational needs of the organization and its long-term strategic goals.
Central to financial governance in healthcare are various leadership roles that directly influence budgeting, cost management, and revenue generation. These roles are typically distributed among several key executives, each with specific responsibilities. They must all work collaboratively to ensure financial health and operational efficiency.
Healthcare middle managers, in roles such as department heads or service-line managers, are also vital to the budgeting process, particularly in larger organizations. These leaders manage specific departments, such as surgery, radiology, supplies, the business office, etc., and are responsible for ensuring their budgets are balanced and aligned with organizational priorities. Department heads must oversee day-to-day expenses, staffing needs, and resource allocation, and they are expected to provide input into the budget by forecasting their department’s expected costs and revenues. They also monitor their department’s performance against financial targets month to month, providing feedback and adjustments as necessary.
In the area of revenue cycle management (RCM), specialized roles like the revenue cycle director or billing manager are responsible for overseeing the process of generating and collecting revenue. These leaders ensure that patient billing is accurate and timely, and that reimbursements from insurers and government programs are maximized. This role includes managing coding accuracy, overseeing the insurance verification process, and ensuring that claims are submitted correctly to avoid costly denials or delays. The revenue cycle team is essential for ensuring that patient billing flows smoothly from registration through to payment, and they work closely with finance teams to ensure that the organization’s cash flow is optimized.
Financial analysts and accountants play an important role in supporting financial governance by providing the necessary data and analysis for decision making. Financial analysts track performance metrics, prepare reports, and conduct financial modeling to forecast revenue and costs. Their work helps executives understand trends, assess financial viability, and make informed decisions regarding budget adjustments, capital investment, and operational strategies. Accountants are responsible for maintaining accurate financial records, ensuring compliance with tax regulations, and assisting with audits and financial reporting.