Table of Contents |
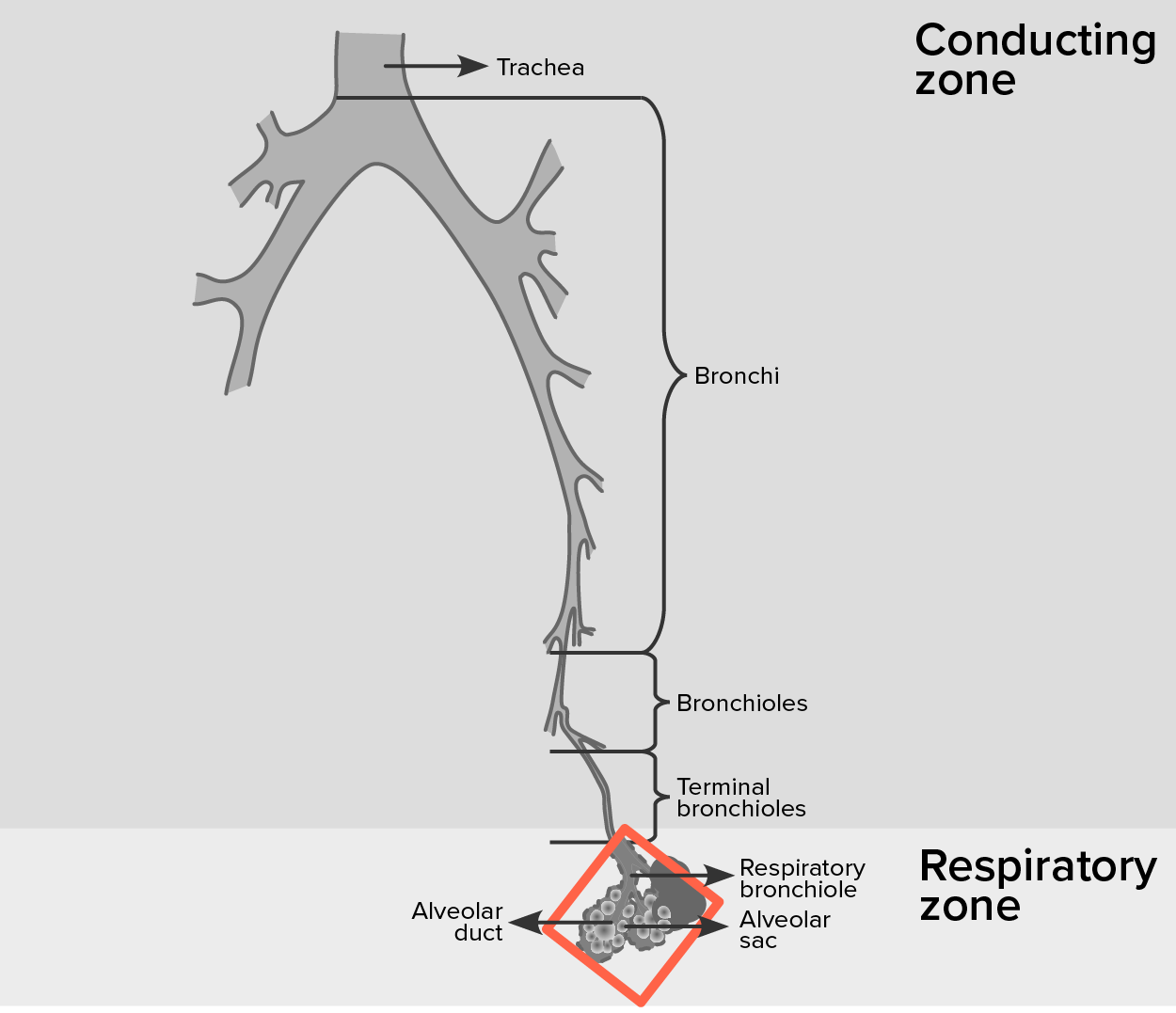
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole, which then leads to an alveolar duct, opening into a cluster of alveoli.
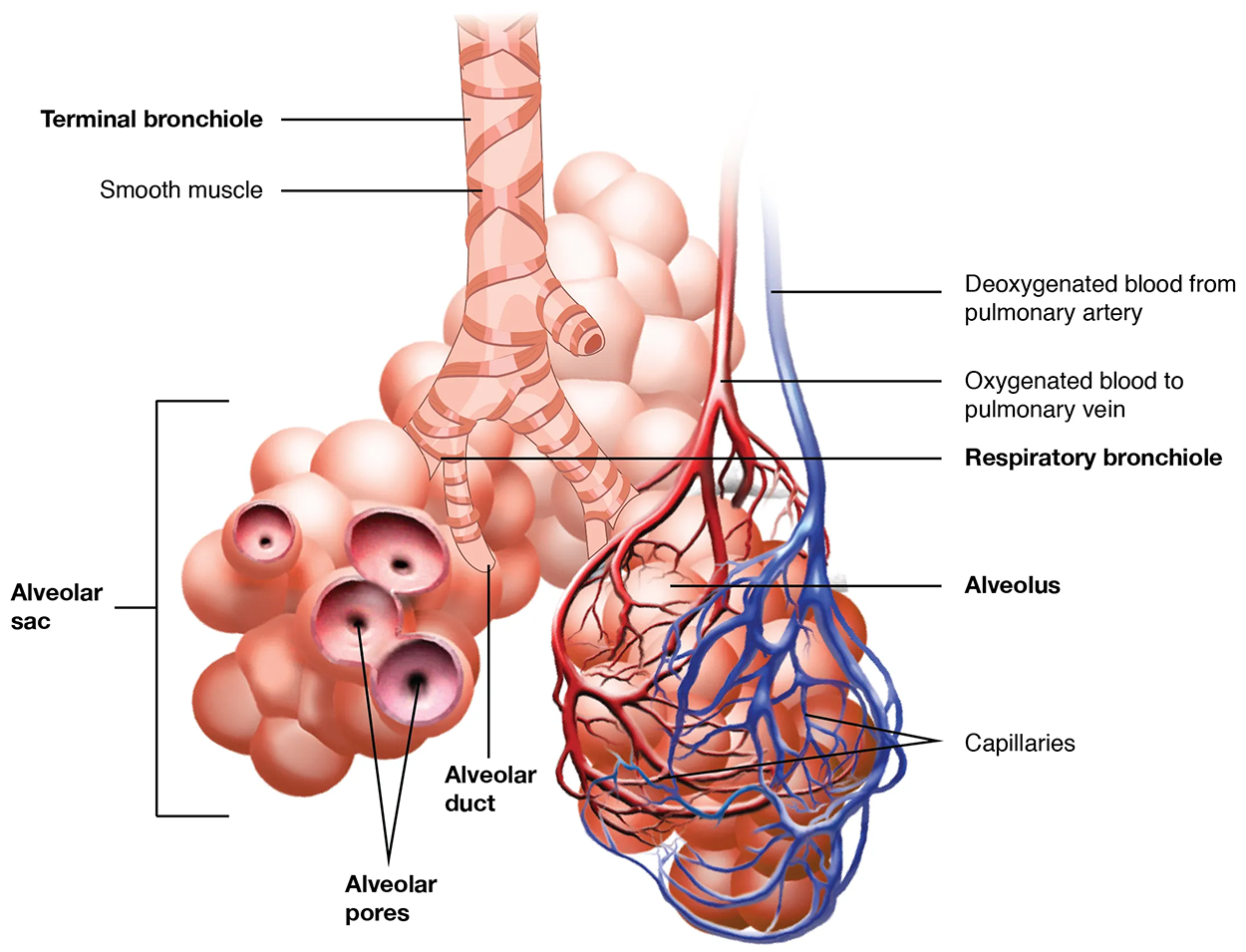
An alveolar duct is a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts and it performs gas exchange in the lungs.
An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange. An alveolus is approximately 200 μm in diameter with elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange. Alveoli are connected to their neighbors by alveolar pores, which help maintain equal air pressure throughout the alveoli and lung.
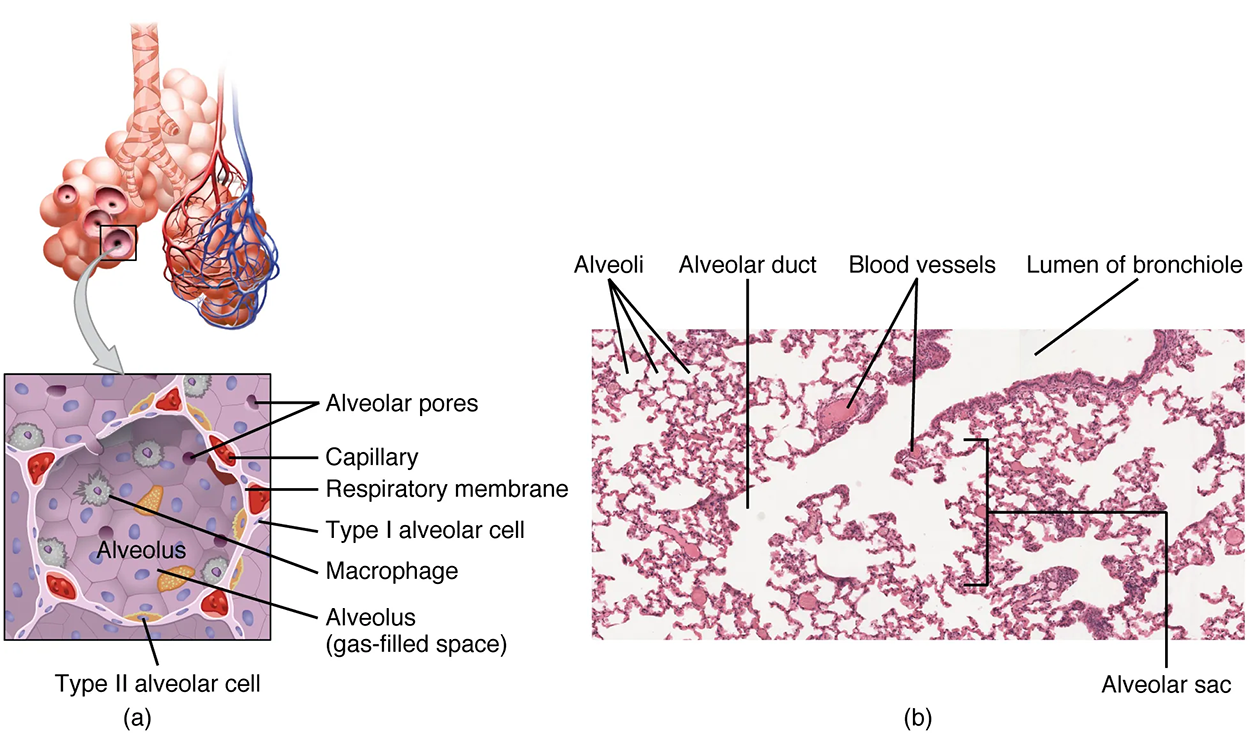
The alveolar wall consists of three major cell types: type I alveolar cells, type II alveolar cells, and alveolar macrophages. A type I alveolar cell is a squamous epithelial cell of the alveoli, which constitutes up to 97% of the alveolar surface area. These cells are about 25 nm thick and are highly permeable to gases. A type II alveolar cell is interspersed among the type I cells and secretes pulmonary surfactant, a substance composed of phospholipids and proteins that reduces the surface tension of the alveoli. Roaming around the alveolar wall is the alveolar macrophage, a phagocytic cell of the immune system that removes debris and pathogens that have reached the alveoli.
The simple squamous epithelium formed by type I alveolar cells is attached to a thin, elastic basement membrane. This epithelium is extremely thin and borders the endothelial membrane of capillaries. Taken together, the alveoli and capillary membranes form a respiratory membrane that is approximately 0.5 μm (micrometers) thick. The respiratory membrane allows gases to cross by simple diffusion, allowing oxygen to be picked up by the blood for transport and CO₂ to be released into the air of the alveoli.
EXAMPLE
| Term | Pronunciation | Audio File |
|---|---|---|
| Alveolus | al·ve·o·lus |
|