Table of Contents |

Small, uncoordinated, and slick with amniotic fluid, a newborn encounters the world outside of the womb. We do not often consider that a child’s birth is proof of the healthy functioning of the reproductive system. Moreover, endocrine systems had to secrete the appropriate regulating hormones to induce the production and release of unique male and female gametes, which are reproductive cells containing genetic material (one set of 23 chromosomes). Reproductive behavior or medical innovation had to facilitate the transfer of male gametes—the sperm—to the female gamete, an oocyte (egg). Finally, the combination of the gametes (fertilization) had to occur, followed by implantation in the uterus and development. In this challenge, you will explore the reproductive system, whose functioning can culminate in the powerful sound of a newborn’s first cry.
As in all animals, the adaptations for reproduction in humans are complex. They involve specialized and different anatomies in the two sexes (males and females), a hormone regulation system, and specialized behaviors regulated by the brain and endocrine system.
Humans reproduce by sexual reproduction, in which the genetic material of two individuals is combined to produce genetically diverse offspring that differ from their parents. The genetic diversity of sexually produced offspring is thought to give species a better chance of surviving in an unpredictable or changing environment. Species that reproduce sexually must maintain two different types of individuals, males and females.
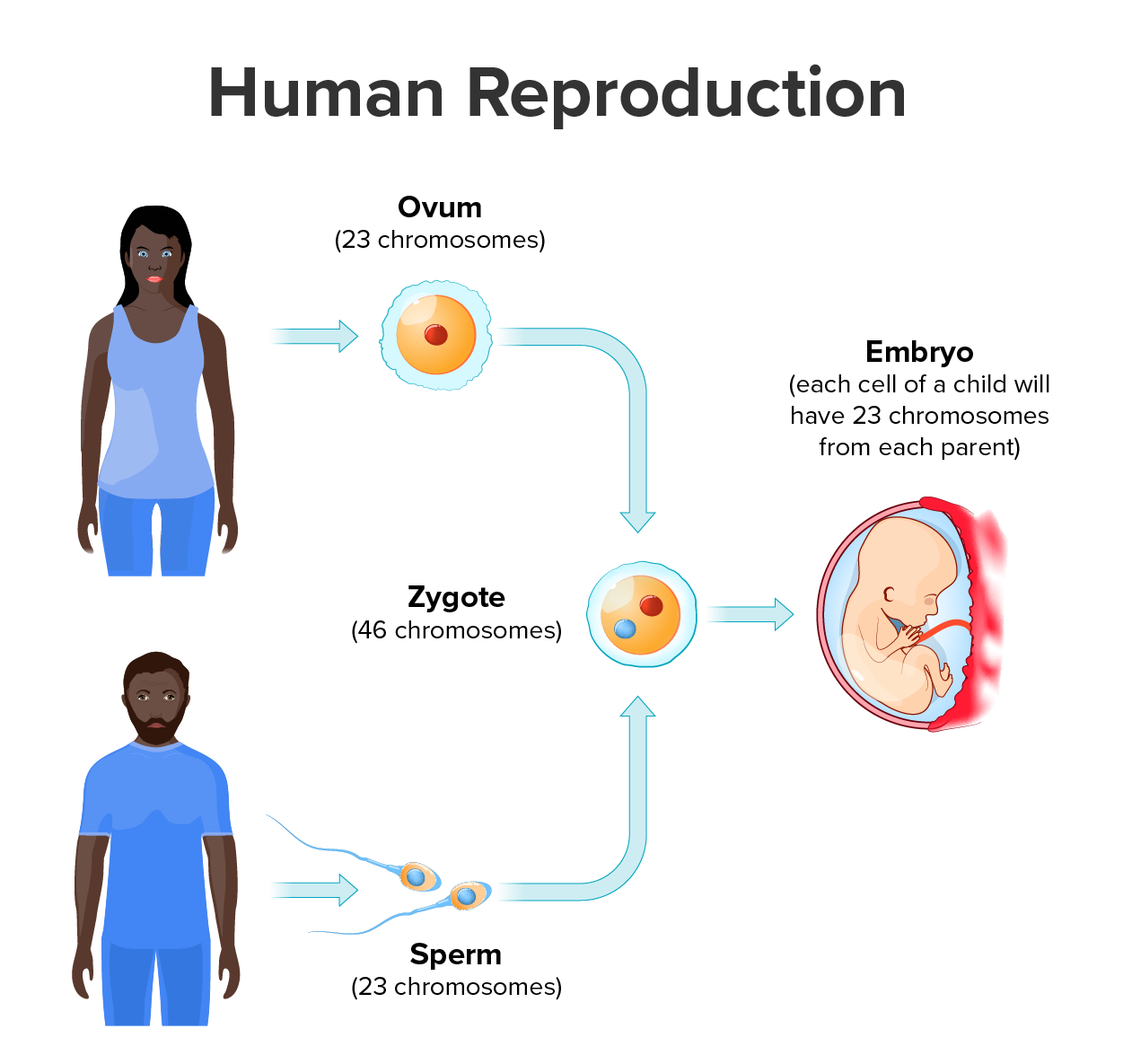
The testes in males and ovaries in females are reproductive organs called gonads that produce gametes and reproductive hormones. Unique for its role in reproduction, a gamete is a specialized sex cell, which in humans carries 23 chromosomes—one-half the number of chromosomes in body cells. In almost all sexually reproducing species, these two haploid cells (cells with one set of chromosomes) differ in size; the smaller gamete is called the male gamete, and the larger one is called the female gamete. Gametogenesis is the formation of gametes: Spermatogenesis is the process of formation of male gametes (sperm), whereas oogenesis is the process of formation of female gametes (ovum). At fertilization, the chromosomes in one sperm (also called a spermatozoon) combine with the chromosomes in one ovum to form a zygote that then develops into an embryo. That embryo grows into a baby.
In the lessons of this challenge, you will learn more about how the human reproductive system facilitates sexual reproduction.
IN CONTEXT
Career Connections: Reproductive Endocrinologist
A reproductive endocrinologist is a physician who treats a variety of hormonal disorders related to reproduction and infertility in people of any gender. The disorders include menstrual problems, infertility, pregnancy loss, sexual dysfunction, and menopause. Doctors may use fertility drugs, surgery, or assisted reproductive techniques (ART) in their therapy. ART involves the use of procedures to manipulate the egg or sperm to facilitate reproduction, such as in vitro fertilization.
Reproductive endocrinologists undergo extensive medical training, first in a 4-year residency in obstetrics and gynecology, then in a 3-year fellowship in reproductive endocrinology. To be board-certified in this area, the physician must pass written and oral exams in both areas.
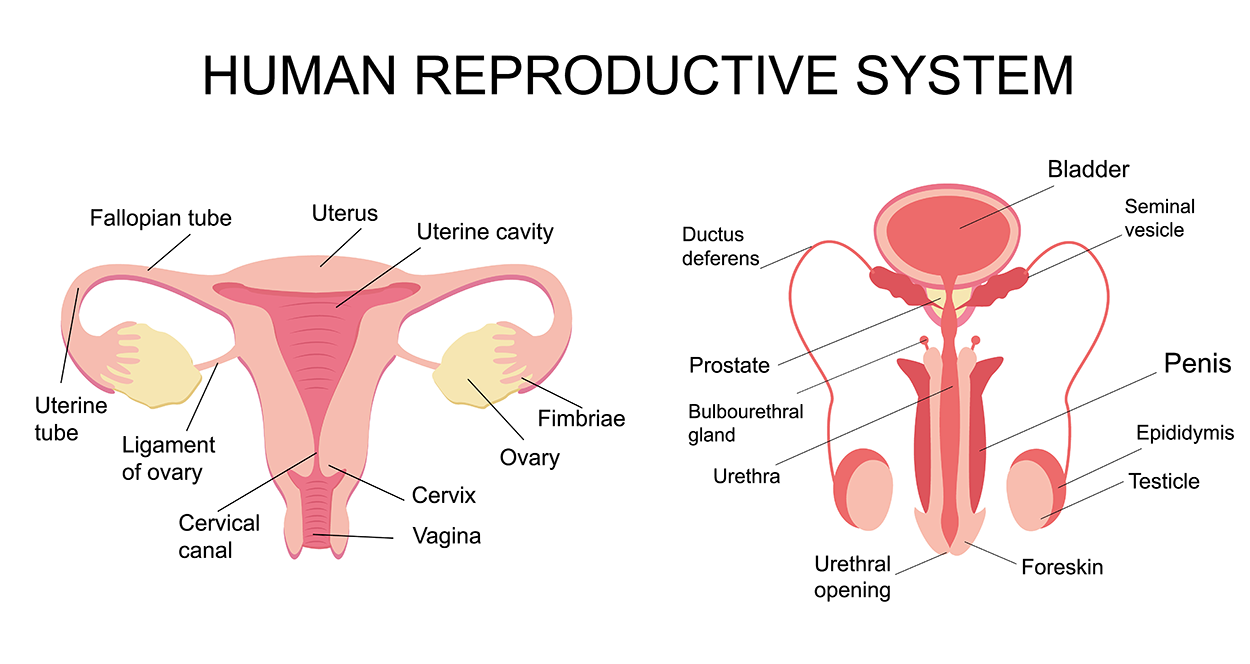
The reproductive tissues of male and female humans develop similarly in utero (in the uterus; before birth) until, in some cases, a low level of the hormone testosterone is released from gonads. Testosterone causes the undeveloped tissues to differentiate into organs, such as the scrotum and penis. When testosterone is absent, the tissues continue to develop into structures such as the ovaries and labia. These cells are considered bipotential: One group of cells has the potential to develop into either type of reproductive structure. Primitive gonads become testes or ovaries. Tissues that produce a penis in males produce a clitoris in females. The tissue that will become the scrotum in a male becomes the labia in a female; that is, they are considered homologous structures (structures that are similar in origin but dissimilar in function).
Males and females also exhibit different characteristics as they develop. Primary sex characteristics are traits that are present at birth that are directly involved in reproduction. These characteristics include structures such as the penis and testes in males and the vagina and ovaries in females.
Puberty is the stage of development at which individuals become sexually mature. Though the outcomes of puberty for different sexes are very different, the hormonal control of the process is very similar. In addition, though the timing of these events varies between individuals, the sequence of changes that occur is predictable for male and female adolescents (a young person developing into an adult).
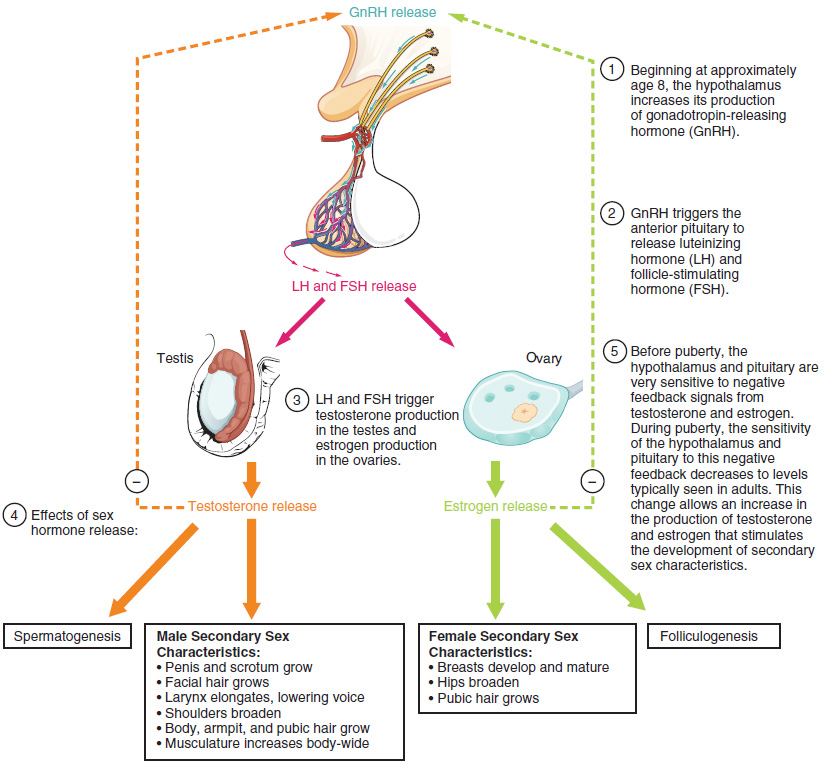
As shown in the figure below, a concerted release of hormones from the hypothalamus (GnRH), the anterior pituitary (LH and FSH), and the gonads (either testosterone or estrogen) is responsible for the maturation of the reproductive systems and the development of secondary sex characteristics, which are physical changes that serve auxiliary (supplementary) roles in reproduction.
Different sex steroid hormone concentrations between the sexes also contribute to the development and function of secondary sexual characteristics. Examples of secondary sexual characteristics are shown below.
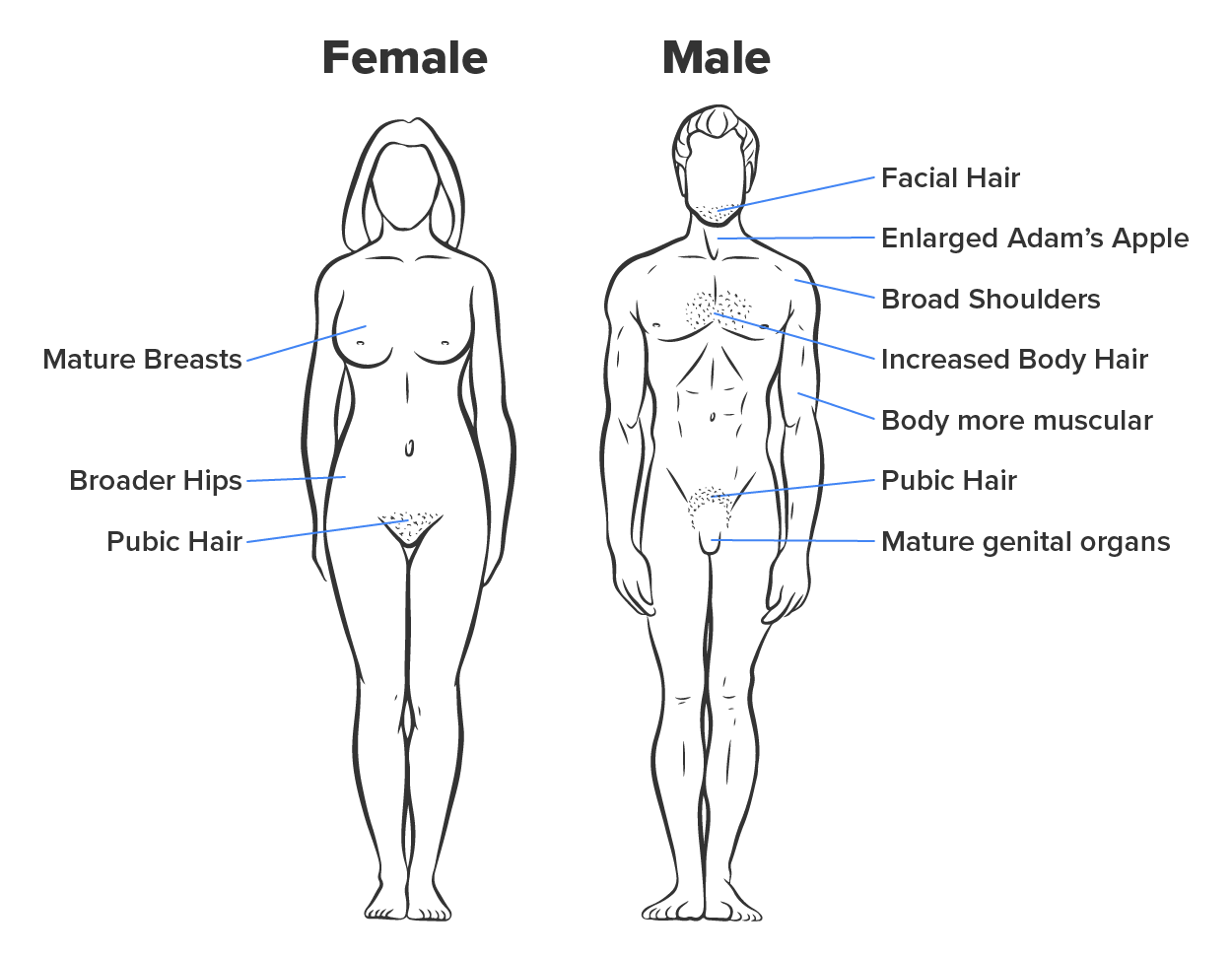
| Development of Secondary Sexual Characteristics | |
|---|---|
| Male | Female |
| Increased larynx size and deepening of the voice | Deposition of fat, predominantly in breasts and hips |
| Increased muscular development | Breast development |
| Growth of facial, axillary, and pubic hair, and increased growth of body hair | Broadening of the pelvis and growth of axillary and pubic hair |
As a female reaches puberty, typically the first change that is visible is the development of the breast tissue. This is followed by the growth of axillary (underarm) and pubic hair. A growth spurt normally starts at approximately age 9 to 11 and may last 2 years or more. During this time, height can increase 3 inches a year. The next step in puberty is menarche, the start of menstruation (the approximately monthly shedding of the inner portion of the endometrium of the uterus through the vagina).
In males, the growth of the testes is typically the first physical sign of the beginning of puberty, which is followed by growth and pigmentation of the scrotum and growth of the penis. The next step is the growth of hair, including armpit, pubic, chest, and facial hair. Testosterone stimulates the growth of the larynx and thickening and lengthening of the vocal folds, which causes the voice to drop in pitch. The first fertile ejaculations typically appear at approximately 15 years of age, but this age can vary widely across individuals. Unlike the early growth spurt observed in females, the male growth spurt occurs toward the end of puberty, at approximately age 11 to 13, and height can increase as much as 4 inches a year. In some males, pubertal development can continue through the early 20s.
The first changes begin around the age of 8 or 9 when the production of LH becomes detectable. The release of LH occurs primarily at night during sleep and precedes the physical changes of puberty by several years. In pre-pubertal children, the sensitivity of the negative feedback system in the hypothalamus and pituitary is very high. This means that very low concentrations of androgens or estrogens will negatively feed back onto the hypothalamus and pituitary, keeping the production of GnRH, LH, and FSH low.
As an individual approaches puberty, two changes in sensitivity occur. The first is a decrease of sensitivity in the hypothalamus and pituitary to negative feedback, meaning that it takes increasingly larger concentrations of sex steroid hormones to stop the production of LH and FSH. The second change in sensitivity is an increase in sensitivity of the gonads to the FSH and LH signals, meaning the gonads of adults are more responsive to gonadotropins than are the gonads of children. As a result of these two changes, the levels of LH and FSH slowly increase and lead to the enlargement and maturation of the gonads, which in turn leads to secretion of higher levels of sex hormones and the initiation of spermatogenesis (the formation of sperm) and folliculogenesis (the development of ovarian follicles into an egg that can be fertilized).
SOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM (1) OPENSTAX “BIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/BIOLOGY-2E/PAGES/1-INTRODUCTION (2) OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION (3) OPENSTAX “CONCEPTS OF BIOLOGY”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/CONCEPTS-BIOLOGY/PAGES/1-INTRODUCTION. LICENSING (1, 2, & 3): CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.