Table of Contents |
Over the past few decades, health information systems have revolutionized healthcare by digitizing patient records and streamlining administrative processes, leading to improved efficiency and accuracy in patient care. These systems have enabled better coordination among providers, reduced human error, and empowered patients with greater access to their health information. In this lesson, you will explore how these systems are designed to improve the delivery of care, enhance operational efficiency, and support decision making.
The adoption of health information systems also contributes to improving public health and safety. These systems can monitor disease outbreaks, track vaccination rates, and analyze trends in healthcare delivery, providing valuable insights for policymakers and healthcare providers. By using HIS, hospitals and clinics can reduce administrative burdens, minimize human error, and optimize patient care. In addition, the data from these systems can be shared across different facilities, promoting better coordination among healthcare providers. Let's explore some specific types of health information systems that assist healthcare managers in their work.
A practice management system (PMS) is a software solution used by physician clinics to handle administrative and business operations. It streamlines tasks like scheduling appointments, billing, patient registration, and managing insurance claims. By automating these processes, a PMS helps reduce administrative workload, minimizes errors, and improves overall clinic efficiency. Clinic staff can quickly access patient information, track payments, and communicate with patients, which boosts productivity and enhances patient satisfaction.
In addition to managing daily operations, a PMS provides valuable reporting and analytics tools. These tools allow clinic managers and physicians to monitor financial performance, track patient flow, and ensure compliance with regulations. By integrating with other healthcare systems like electronic health records (EHR), the practice management system ensures smooth coordination between administrative and clinical functions, leading to better patient care and operational success.
IN CONTEXT
Junie, a medical office administrator, begins their day by logging into the practice management system (PMS), where they review the schedule for the day. The system displays a list of appointments, showing patient names, times, and any special requirements, such as whether the patient needs to complete specific paperwork. Then, Junie verifies if any patient has recently updated their insurance information or personal details, ensuring everything is current before they arrive. When a patient checks in for their appointment, Junie quickly pulls up their profile in the PMS, confirming their details and collecting any co-pays or outstanding balances.
Throughout the day, Junie manages phone calls and appointment requests using the PMS’s scheduling feature. If a patient needs to reschedule, Junie checks the doctor’s availability and makes adjustments directly in the system, automatically updating the schedule. For new patients, Junie enters their information into the system, which then populates relevant forms and starts the billing process. When the patient’s visit concludes, Junie uses the PMS to generate a claim that is submitted electronically.
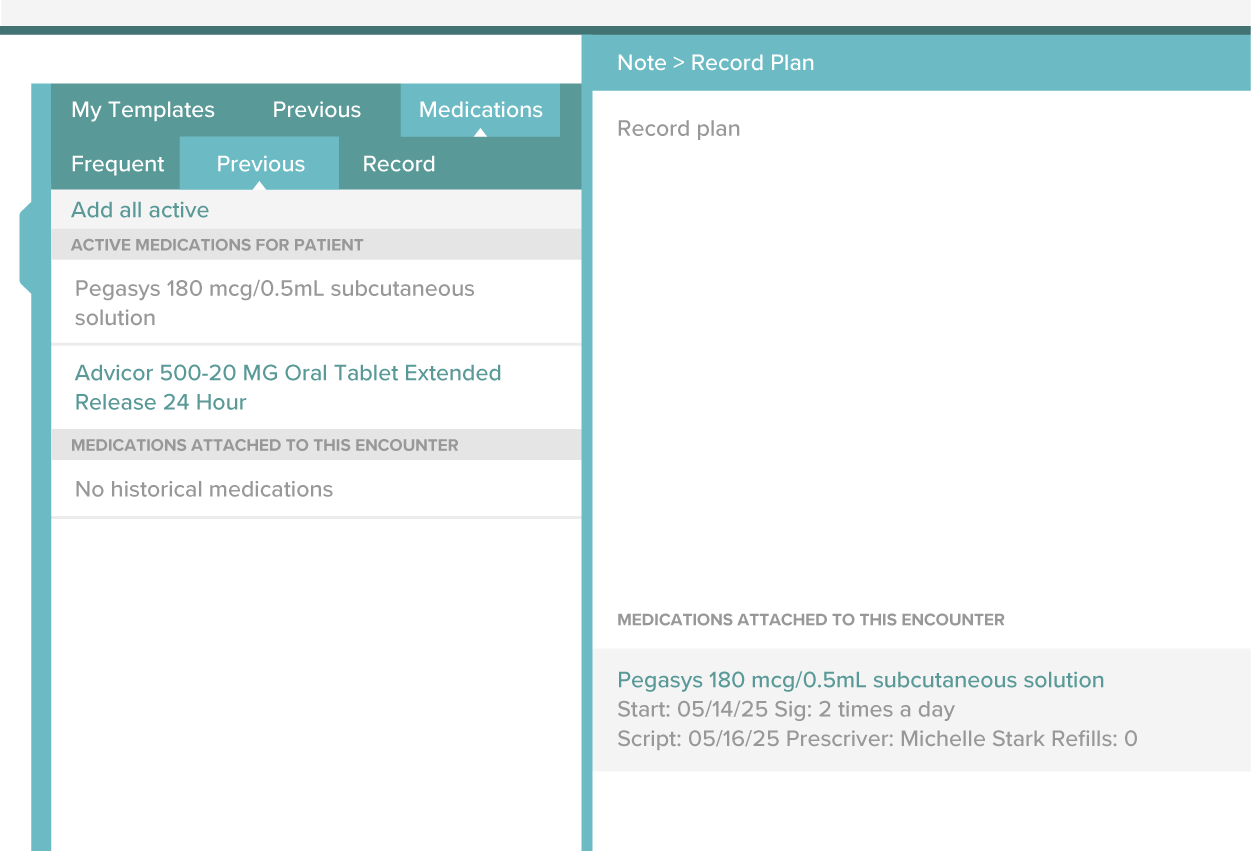
Electronic health records (EHR) are digital versions of a patient’s chart that were previously kept on paper, storing comprehensive health information in one secure system. EHRs include details such as medical history, diagnoses, medications, allergies, lab results, immunization status, and treatment plans. They allow healthcare providers to access and update patient information in real time, making it easier to coordinate care and make informed decisions. EHR systems can be shared across different healthcare settings so that specialists, labs, and pharmacies can all access the same information, leading to better communication and more efficient care.
Clinical decision support systems (CDSS) are computerized tools that assist healthcare providers in making clinical decisions by analyzing patient data and offering evidence-based recommendations, alerts, or reminders to improve care outcomes. They are another important function of HIS. These systems integrate with electronic health records (EHRs) to evaluate clinical data, such as lab results, medical history, and current symptoms, and offer suggestions that improve diagnosis, treatment, and patient outcomes. CDSS can alert clinicians to potential issues like drug interactions, allergies, or deviations from clinical guidelines, ensuring safer and more effective care. By supporting decision making in real time, CDSS helps reduce errors, enhance clinical workflows, and ultimately contributes to higher quality patient care.
EXAMPLE
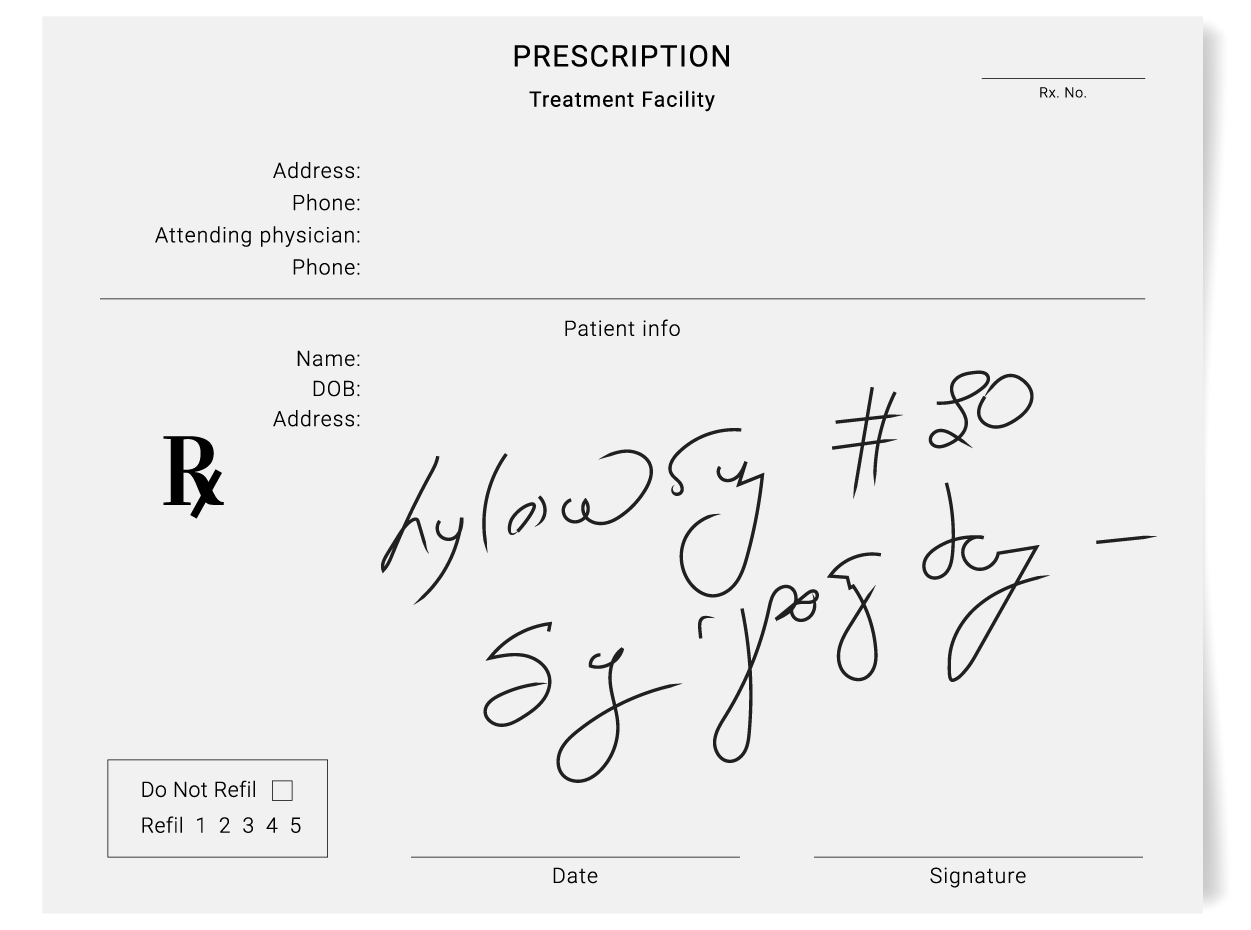
Dr. Sharma is working in the EHR, documenting his latest observations and prescriptions for his patient. A pop-up bubble appears on the screen that says: "Alert: The patient’s prescription for Warfarin may interact with their current antibiotic, Ciprofloxacin. Please review and consider adjusting the medication regimen to prevent potential bleeding complications."Order entry management is a key function of health information systems that streamlines the process of ordering tests, medications, and treatments. Computerized physician order entry (CPOE) is a system that allows healthcare providers to electronically enter and manage orders, such as prescriptions, lab tests, imaging requests, and other medical instructions. The primary purpose of CPOE is to streamline and automate the ordering process, reducing the need for handwritten orders which are often difficult to read and can lead to errors. By digitizing the ordering process, CPOE improves accuracy, enhances efficiency, and accelerates the delivery of care, allowing clinicians to quickly access and process orders within the electronic health record (EHR) system.
Health information systems are crucial for managing administrative tasks in healthcare by automating processes that assist with the operations of a healthcare organization. These systems enable healthcare facilities to track appointments, verify patient information, track inventory, and manage financial transactions efficiently. Just like with the practice management system (PMS) reviewed earlier, administrative systems can schedule appointments, send reminders to patients, and streamline the billing process by generating invoices and submitting insurance claims electronically. Additionally, health information systems can help monitor and manage staffing, track inventory, and ensure compliance with regulations. All of these applications assist healthcare managers in doing their job more efficiently. It gives them data and reports as needed, which can help with planning and decision making. HIS can help the CFO and accountants by enabling them to track the finances of all areas of a healthcare system and monitor the financial health of the organization.
Inventory and supply chain management is a critical function of HIS. Because healthcare facilities rely on a reliable stock of medical supplies, medications, and equipment, HIS is used to track the inventory and trigger an alert when a supply is getting low. It can then assist with the ordering process as well. By monitoring inventory levels in real time, hospitals can ensure that they have the necessary resources to provide care without overstocking or running out of essential items.
As mentioned, HIS makes it easy for healthcare managers to pull reports. Reporting and analytics are vital functions that provide insights into hospital operations and patient outcomes. HIS can generate reports on various metrics, such as patient satisfaction, treatment success rates, and financial performance. These reports help hospital administrators identify areas for improvement and make data-driven decisions.
EXAMPLE
The analytics at South Medical Center reveal a high rate of patient readmissions. This drives the chief of staff and nursing manager of the hospital to investigate the underlying causes and implement strategies to improve patient care and reduce readmissions.In the past few decades, the electronic health record (EHR) has been one of the biggest changes to healthcare management in the history of healthcare in the U.S. The evolution of the EHR has been shaped by technological advancements, regulatory changes, and the growing demand for more efficient, accurate, and accessible healthcare. The journey began in the 1960s, when the first attempts to digitize medical data were made, although these early systems were primarily focused on laboratory data and administrative tasks rather than comprehensive patient records. By the 1970s and 1980s, computer systems began to gain traction in hospitals and clinics, with some institutions experimenting with basic and simplistic electronic systems to manage patient information, but widespread adoption was limited due to high costs and technology limitations.
The 1990s marked the shift toward more integrated and comprehensive electronic systems, driven by the increasing need to streamline patient care, reduce errors, and improve operational efficiency. The concept of the EHR began to take shape, emphasizing the electronic storage of patient health data, including medical history, diagnoses, treatments, medications, and test results. However, challenges still existed in interoperability (the ability of different systems, devices, or applications to work together, exchange data, and use that data effectively across various platforms or organizations), with different systems unable to communicate with each other. This hindered the exchange of patient information across healthcare providers.
The early 2000s saw significant momentum in EHR development, especially in the United States, with the introduction of policies to incentivize adoption. In 2004, President George W. Bush established the Office of the National Coordinator for Health Information Technology (ONC) to promote the use of health IT. This initiative helped lay the groundwork for widespread EHR adoption, culminating in the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009. This legislation provided financial incentives to healthcare providers who demonstrated their use of EHRs, driving rapid adoption across the healthcare sector. By this time, EHRs had become more sophisticated, with features like e-prescribing, clinical decision support, and the ability to integrate with other health information systems.
IN CONTEXT
Office of the National Coordinator for Health Information Technology (ONC)
In 2004, President George W. Bush established this office to promote the use of information technology in healthcare.
Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009
This key piece of legislation in the United States was designed to accelerate the adoption of health information technology (IT) and improve healthcare quality through the use of electronic health records (EHR) and other digital tools. It provided financial incentives to healthcare providers and hospitals to encourage the meaningful use of EHR systems.
As adoption expanded, the focus shifted toward improving the functionality, usability, and interoperability of EHR systems. Efforts were made to standardize data formats and improve communication between different systems to ensure the seamless sharing of patient information across healthcare settings. By the 2010s, EHRs had become a cornerstone of modern healthcare. Not only did they streamline administrative tasks, such as billing and scheduling, but they also enhanced patient care by providing healthcare providers with comprehensive, up-to-date patient information at the point of care. Patient portals emerged, allowing individuals to access their health records, schedule appointments, and communicate with providers more easily.
The patient portal emerged as part of the broader movement toward digitizing healthcare and empowering patients to take a more active role in managing their health. As EHRs became widely adopted, healthcare providers saw an opportunity to offer patients secure, online access to their personal health information. The development of patient portals gained significant momentum in the 2000s, particularly with the encouragement of government initiatives like the HITECH Act, which incentivized the meaningful use of EHRs and included patient access to their medical records as a key component. The portal became a tool for improving communication between patients and healthcare providers while increasing transparency and engagement in health management.
Today, patient portals are used for a wide range of functions. Patients can log in securely to view their test results, track appointments, request prescription refills, and even message their healthcare providers. They can access their medical history, immunization records, and billing information, allowing them to manage their healthcare more efficiently.
Artificial intelligence (AI) is increasingly being integrated into healthcare to improve diagnostics, enhance treatment plans, and streamline administrative processes. In clinical settings, AI algorithms analyze medical images such as X-rays, MRIs, and CT scans, assisting radiologists in detecting conditions like cancer, fractures, and other abnormalities with greater accuracy and speed. AI is also being used in predictive analytics to assess patient risks, identify early signs of diseases like heart disease or diabetes, and predict patient outcomes, allowing healthcare providers to intervene earlier. Machine learning models can process vast amounts of data to recognize patterns that may be overlooked by human providers, improving decision making and enabling more personalized treatment approaches.
AI is also transforming administrative tasks within healthcare organizations, automating routine activities like scheduling, billing, and patient triage. Furthermore, AI-driven chatbots and virtual assistants are helping patients manage appointments, receive reminders for medication, and answer basic health inquiries, improving patient engagement.
Source: THIS TUTORIAL WAS AUTHORED BY SOPHIA LEARNING. PLEASE SEE OUR TERMS OF USE.