Table of Contents |
Filtration is the first step in urine production, and this part of urine formation ensures that only necessary products are excreted from the body.
Filtration only occurs within a specific part of the nephron, the Bowman's capsule. During filtration, blood enters the capillaries within the Bowman's capsule, called the glomerulus (plural, glomeruli), through the afferent arteriole, which is narrow compared to other blood vessels within the body. Because of this, blood is delivered towards the nephron through the afferent arteriole at high pressure due to the narrower diameter. This high pressure forces water and solutes from the blood in these afferent arterioles into the Bowman's capsule of the nephron.
The solutes that are forced out of the blood include glucose, sodium, urea, vitamins, amino acids, et cetera. Water and solutes that are pushed out of the blood would then flow into the proximal tubule, where the next stage of urine formation occurs: reabsorption.
The rates of filtrate volume formation and filtration through the kidney are described in the subsections below.
The volume of filtrate formed by both kidneys per minute is termed the glomerular filtration rate (GFR). The heart pumps about 5 liters (L) of blood per min under resting conditions. Approximately 20% (1 L) enters the kidneys to be filtered. On average, this liter results in the production of about 125 milliliters (mL)/minute (min) filtrate produced in males (range of 90 to 140 mL/min) and 105 mL/min filtrate produced in females (range of 80 to 125 mL/min). This amount equates to a volume of about 180 L/day in males and 150 L/day in females. Approximately 99% of this filtrate is returned to the circulation by reabsorption so that only about 1–2 L of urine are produced per day (see the table below for how to calculate urine formation).
| Calculating Urine Formation Per Day | ||
|---|---|---|
| Flow per minute (mL) | Calculation | |
| Renal blood flow | 1050 |
Cardiac output is about 5000 mL/minute, of which 21% flows through the kidney. 5000 × 0.21 = 1050 mL blood/min |
| Renal plasma flow | 578 |
Renal plasma flow equals the blood flow per minute times the hematocrit. If a person has a hematocrit of 45, then the renal plasma flow is 55%. 1050 × 0.55 = 578 mL plasma/min |
| Glomerular filtration rate | 110 |
The GFR is the amount of plasma entering Bowman’s capsule per minute. It is the renal plasma flow times the fraction that enters the renal capsule (19%).
578 × 0.19 = 110 mL filtrate/min |
| Urine | 1296 mL/day |
The filtrate not recovered by the kidney is the urine that will be eliminated. It is the GFR times the fraction of the filtrate that is not reabsorbed (0.8%).
110 × .008 = 0.9 mL urine/min Multiply urine/min times 60 minutes times 24 hours to get daily urine production. 0.9 × 60 × 24 = 1296 mL/day urine |
Determination of the GFR is one of the tools used to assess the kidney’s excretory function, and this is more than just an academic exercise. Because many drugs are excreted in the urine, a decline in renal function can lead to toxic accumulations. Additionally, administration of appropriate drug dosages for those drugs primarily excreted by the kidney requires an accurate assessment of GFR.
GFR can be estimated closely by intravenous administration of inulin. Inulin is a plant polysaccharide that is neither reabsorbed nor secreted by the kidney. Its appearance in the urine is directly proportional to the rate at which it is filtered by the renal corpuscle; the clearance rate for a given substance equals the GFR when it is neither secreted nor reabsorbed by the kidneys.
GFR can be calculated by this equation as well:
GFR = [UrineX (mg/mL)] × urine flow (mL/min) / [PlasmaX (mg/mL)]
The variable X is a substance that is excreted (Shahbaz & Gupta, 2023).
However, because measuring inulin clearance (the volume of urine that is cleared of inulin, which is the same amount of urine that is filtered) is cumbersome in the clinical setting, most often, the GFR is estimated by measuring naturally occurring creatinine, a protein-derived molecule produced by muscle metabolism that is not reabsorbed and only slightly secreted by the nephron.
Creatinine clearance involves measuring the concentration in the blood and urine. The urine is collected over a 5–8 hour period, and the volume of urine is divided by the time to get the urine flow. From the measurements of plasma creatinine, urine creatinine, and urine flow, GFR can be approximated. Creatinine clearance will be slightly higher than actual GFR because the peritubular capillaries secrete some creatinine into the filtrate.
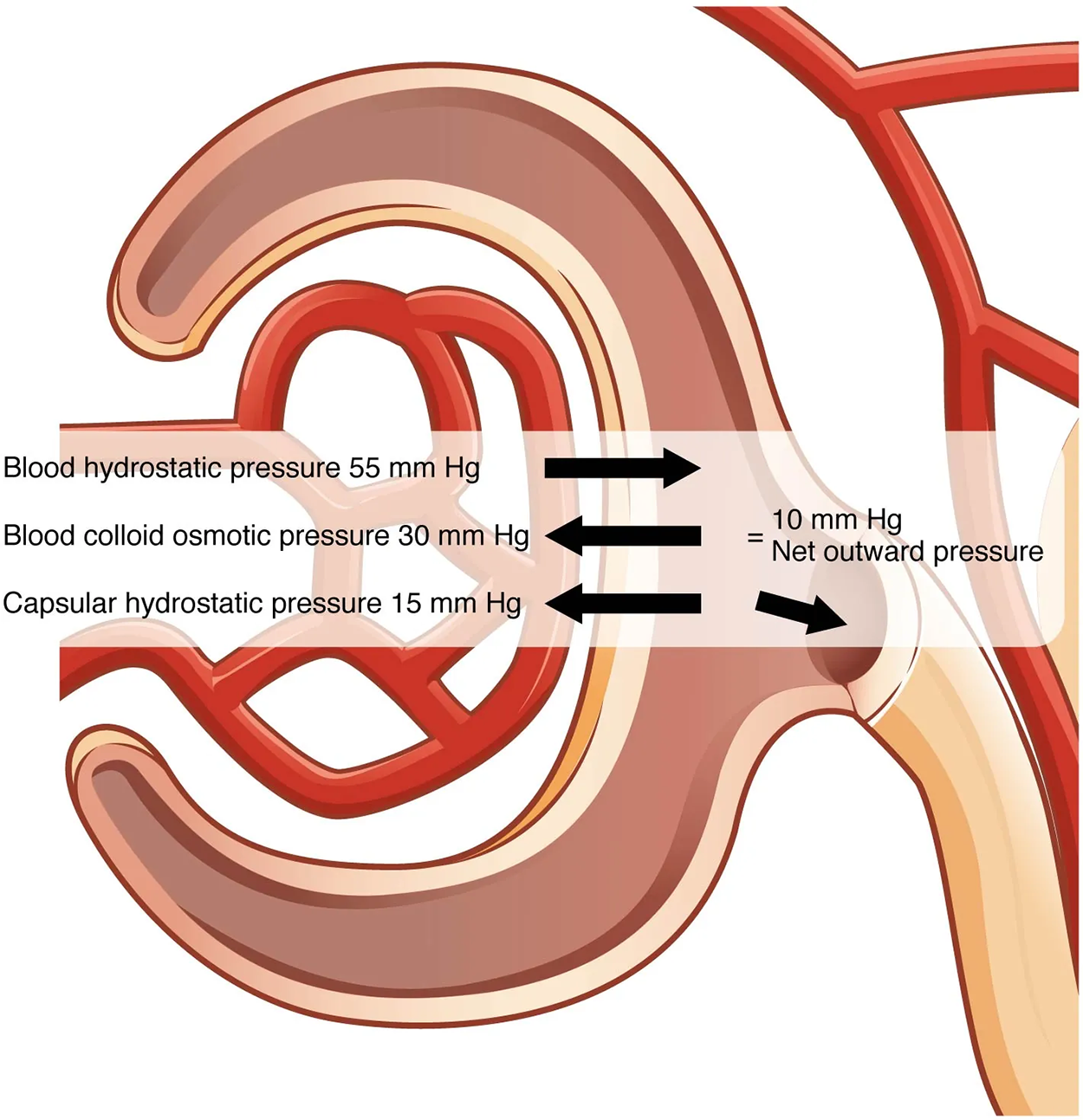
The absence of proteins in Bowman’s space (the lumen within Bowman’s capsule) results in an osmotic pressure near zero. Thus, the only pressure moving fluid across the capillary wall into the lumen of Bowman’s space is hydrostatic pressure. Hydrostatic pressure is sufficient to push water through the membrane despite the osmotic pressure working against it. The sum of all of the influences, both osmotic and hydrostatic, results in a net filtration pressure (NFP) of about 10 mm Hg.
IN CONTEXT
A proper concentration of solutes in the blood is important in maintaining osmotic pressure both in the glomerulus and systemically. There are disorders in which too much protein passes through the filtration slits into the kidney filtrate. This excess protein in the filtrate leads to a deficiency of circulating plasma proteins. In turn, the presence of protein in the urine increases its osmolarity; this holds more water in the filtrate and results in an increase in urine volume. Because there is less circulating protein, principally albumin, the osmotic pressure of the blood falls. Less osmotic pressure pulling water into the capillaries tips the balance towards hydrostatic pressure, which tends to push it out of the capillaries. The net effect is that water is lost from the circulation to interstitial tissues and cells. This “plumps up” the tissues and cells, a condition termed systemic edema.
NFP determines filtration rates through the kidney. It is determined as follows:
NFP = Glomerular blood hydrostatic pressure (GBHP) – [capsular hydrostatic pressure (CHP) + blood colloid osmotic pressure (BCOP)] = 10 mm Hg
That is:
NFP = 55 – [15 + 30] = 10 mm Hg
As you can see, there is a low net pressure across the filtration membrane. Minor changes in the osmolarity of the blood or changes in capillary blood pressure result in major changes in the amount of filtrate formed at any given point in time.
The kidney is able to cope with a wide range of blood pressures. In large part, this is due to the autoregulatory nature of smooth muscle. When you stretch it, it contracts. Thus, when blood pressure goes up, smooth muscle in the afferent capillaries contracts to limit any increase in blood flow and filtration rate. When blood pressure drops, the same capillaries relax to maintain blood flow and filtration rate. The net result is a relatively steady flow of blood into the glomerulus and a relatively steady filtration rate in spite of significant systemic blood pressure changes.
GBHP is difficult to measure in a clinical setting, so mean arterial pressure (MAP) can be used. MAP is calculated by adding 1/3 of the difference between the systolic and diastolic pressures to the diastolic pressure. Therefore, if the blood pressure is 110/80, the difference between systolic and diastolic pressure is 30. One-third of this is 10, and when you add this to the diastolic pressure of 80, you arrive at a calculated MAP of 90 mm Hg. Therefore, if you use MAP for the GBHP in the formula for calculating NFP, you can determine that as long as MAP is above approximately 60 mm Hg, the pressure will be adequate to maintain glomerular filtration.
Filtration fraction (FF) is another measure of kidney function. FF is the amount of renal plasma flow (RPF) that gets filtered across the glomerulus. This is calculated by dividing GFR by RPF. FF is usually around 20%, and the other 80% of renal plasma continues its pathway through renal circulation.
Increased FF indicates that there is increased protein concentration of the peritubular capillaries. This leads to additional absorption in the proximal tubule. However, decreased FF results in a decreased amount of fluid that is filtered across the glomerulus per unit of time. Downstream in the peritubular vessels, there is decreased protein concentration, and there is also lessened absorptive capacity of the proximal tubules.
Recall that the afferent and efferent arterioles are two resistance vessels. When blood pressure drops (e.g., because of hemorrhagic shock), sympathetic outflow increases. Both sets of arterioles then vasoconstrict. This keeps the FF constant in the face of decreasing blood pressure.
 Interactive 3-D Model
Interactive 3-D ModelSOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION. LICENSE: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.
REFERENCES
Shahbaz H, Gupta M. Creatinine Clearance. [Updated 2023 May 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: ncbi.nlm.nih.gov/books/NBK544228/
Gounden V, Bhatt H, Jialal I. Renal Function Tests. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from:ncbi.nlm.nih.gov/books/NBK507821/