Table of Contents |
One of the most talked about diseases is skin cancer. Recall that cancer is uncontrolled cell division in which the growing cells have invaded and pose a threat to surrounding tissues. Most cancers are identified by the organ or tissue in which the cancer originates, such as skin cancer.
The Skin Cancer Foundation reports that one in five Americans will experience some type of skin cancer in their lifetime. Overexposure to ultraviolet (UV) radiation damages DNA, which can lead to the formation of cancerous lesions. A lesion is part of an organ or tissue that has been damaged by injury or disease. Although melanin offers some protection against DNA damage from the sun, often it is not enough. The fact that cancers can also occur on areas of the body that are normally not exposed to UV radiation suggests that there are additional factors that can lead to cancerous lesions.
In general, cancers result from an accumulation of DNA mutations. These mutations can result in cell populations that do not die when they should and uncontrolled cell proliferation that leads to tumors. Although many tumors are benign (harmless), some produce cells that can mobilize and establish tumors in other organs of the body; this process is referred to as metastasis. Cancers are characterized by their ability to metastasize.
Basal cell carcinoma is a form of cancer that affects the mitotically active stem cells in the stratum basale of the epidermis. It is the most common of all cancers that occur in the United States and is frequently found on the head, neck, arms, and back—which are areas that are most susceptible to long-term sun exposure. Although UV rays are the main culprit, exposure to other agents, such as radiation and arsenic, can also lead to this type of cancer. Basal cell carcinomas start in the stratum basale and usually spread along this boundary. At some point, they begin to grow toward the surface and become an uneven patch, bump, growth, or scar on the skin's surface. Like most cancers, basal cell carcinomas respond best to treatment when caught early. Treatment options include surgery, freezing (cryosurgery), and topical ointments (Mayo Clinic, 2012).

Squamous cell carcinoma is a cancer that affects the keratinocytes of the stratum spinosum and presents as lesions commonly found on the scalp, ears, and hands. It is the second most common skin cancer, and it is more aggressive than basal cell carcinoma. If not removed, these carcinomas can metastasize.

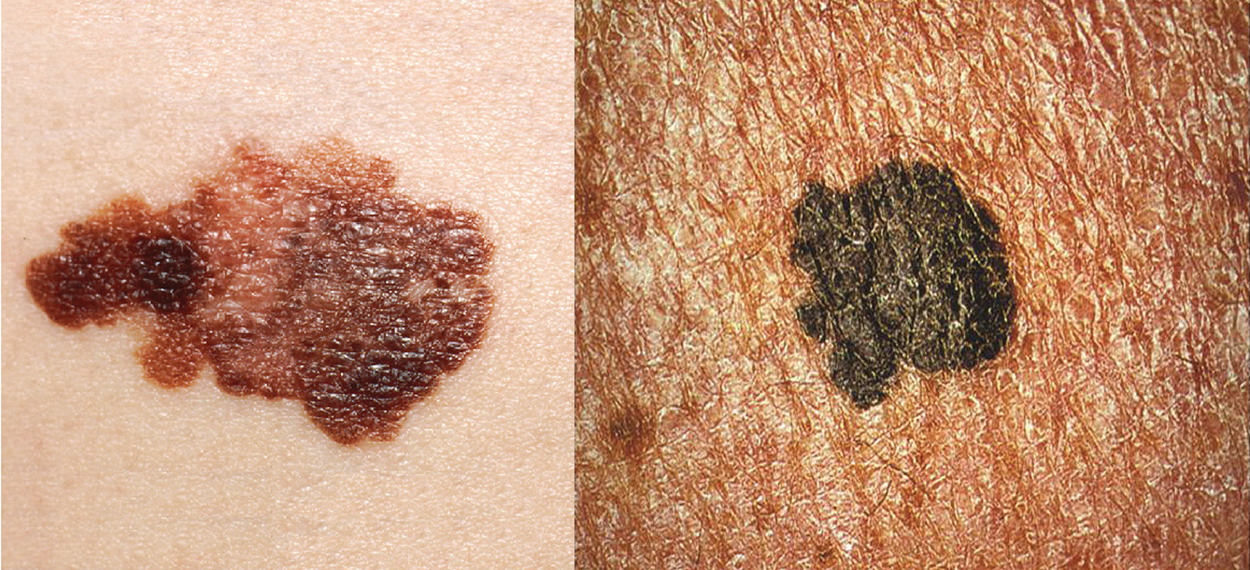
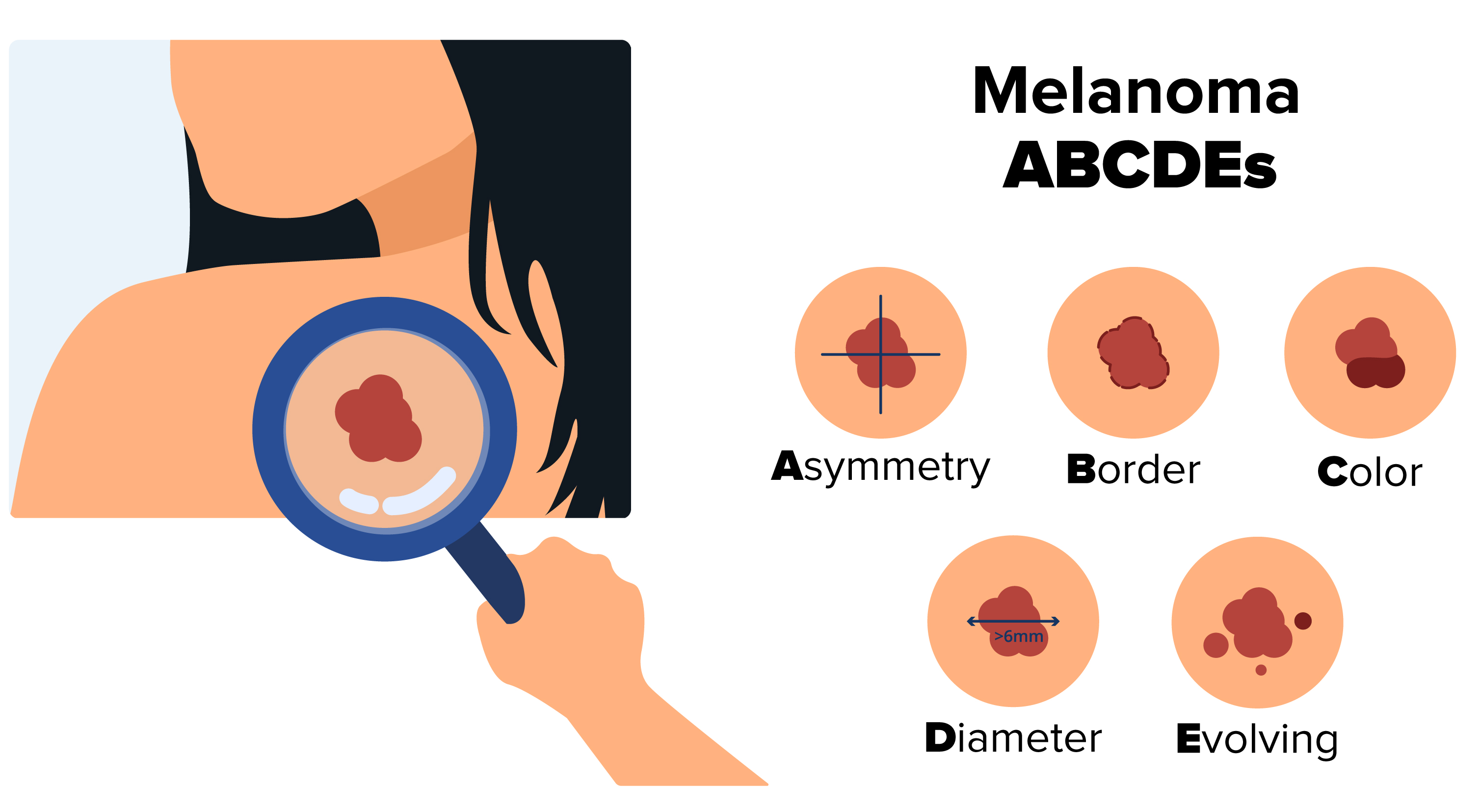
A melanoma is a cancer characterized by the uncontrolled growth of melanocytes, the pigment-producing cells in the epidermis. Typically, a melanoma develops from a mole. It is the most fatal of all skin cancers, as it is highly metastatic and can be difficult to detect before it has spread to other organs. Melanomas usually appear as asymmetrical brown and black patches with uneven borders and a raised surface. Treatment typically involves surgical excision and immunotherapy, which is a type of therapy that stimulates or suppresses the body’s immune response.
Two common skin disorders are eczema and acne. Eczema is an inflammatory condition and occurs in individuals of all ages. Acne involves the clogging of pores, which can lead to infection and inflammation and is often seen in adolescents. Some other disorders that are not discussed here include seborrheic dermatitis (on the scalp), psoriasis, cold sores, impetigo, scabies, hives, and warts.
Eczema is an allergic reaction that manifests as dry, itchy patches of skin that resemble rashes. It may be accompanied by swelling of the skin, flaking, and in severe cases, bleeding. Many who suffer from eczema have antibodies against dust mites in their blood, but the link between eczema and allergy to dust mites has not been proven. Symptoms are usually managed with moisturizers, corticosteroid creams, and immunosuppressants.

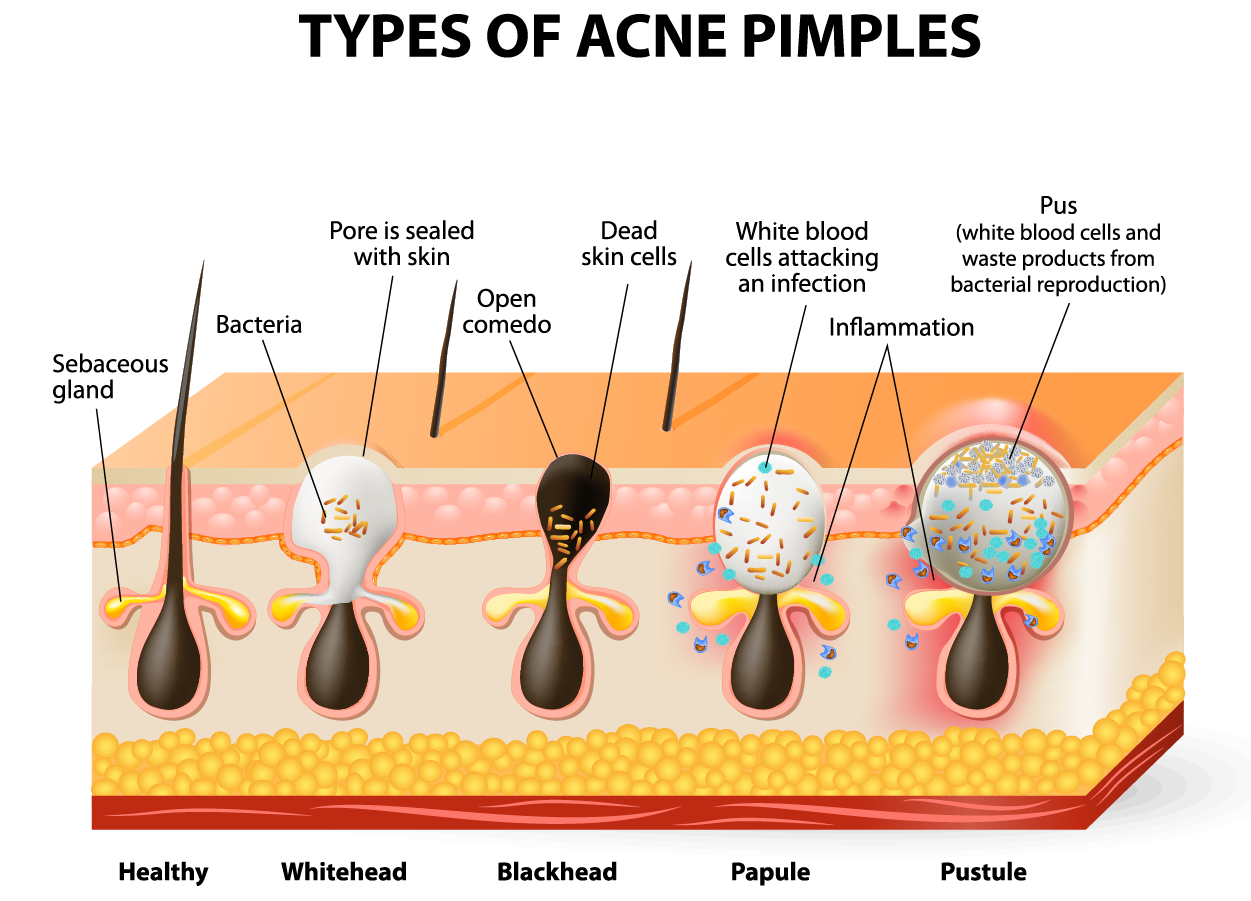
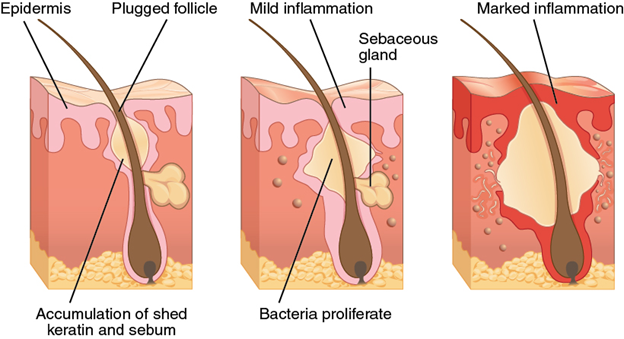
Acne is a skin disorder in which a sebaceous gland becomes infected by acne-causing bacteria (Propionibacterium and Staphylococcus). It is most common along with the onset of puberty because of associated hormones that control sebum production, but it can also occur in infants and continue into adulthood. An overproduction and accumulation of sebum along with dead skin cells can cause hair follicles to become blocked. This plug is initially white because of the natural color of sebum and is commonly called a whitehead. The sebum, when oxidized by exposure to air, turns black and is commonly called a blackhead.
The skin contains plenty of bacteria, most of which are harmless to the body. When a sebaceous gland is blocked, the bacteria within this temporarily enclosed space release chemicals that signal for inflammation in the body. Inflammation brings in extra blood and cells, increasing pressure inside this enclosed space and turning the skin surface red. At this point, the inflamed sebaceous gland is called a papule. As bacteria multiply, blood cells kill bacteria and pus accumulates. The pimple, now called a pustule, continues to increase in size, redness, and pressure on surrounding nerves, causing sensations of pain.
For most, acne decreases after puberty due to a decrease in hormones. During puberty, or for those in puberty, a range of practices such as regular skin cleaning, over-the-counter or prescription topical creams, and even oral medications are available.
As noted above, acne results from infection by acne-causing bacteria. This can lead to redness and potential scarring due to the natural wound healing process.
IN CONTEXT
Career Connection—Dermatologist
Have you ever had a rash that did not respond to over-the-counter creams or a mole that you were concerned about? Dermatologists help patients with these types of problems and more. Dermatologists are medical doctors who specialize in diagnosing and treating skin disorders.
Like all medical doctors, dermatologists earn a medical degree, complete a varying number of additional years of training depending on their specialty, and must obtain official licenses and certifications before working in the United States.
Most dermatologists work in a medical office or private practice setting. They diagnose skin conditions and rashes, prescribe oral and topical medications to treat skin conditions, and may perform simple procedures, such as mole or wart removal. In addition, they may refer patients to an oncologist (a medical professional who specializes in cancer diagnostics and treatment) if skin cancer that has metastasized is suspected.
Recently, cosmetic procedures have also become a prominent part of dermatology. Botox injections, laser treatments, and collagen and dermal filler injections are popular among patients.
Consider visiting a dermatologist to talk about why they entered the field and what the field of dermatology is like.
Because the skin is the part of our bodies that meets the world most directly, it is especially vulnerable to injury. Injuries include burns and wounds, as well as scars and calluses. They can be caused by sharp objects, heat, or excessive pressure or friction to the skin.
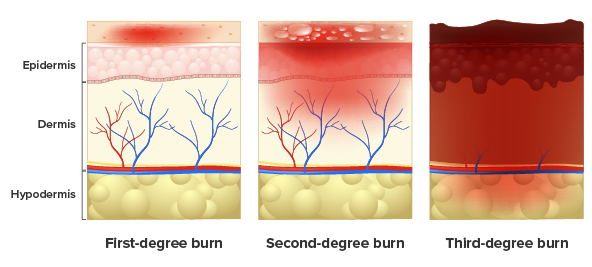
A burn results when the skin is damaged by intense heat, radiation, electricity, or chemicals. The damage results in the death of skin cells, which can hinder skin function. If serious, a burn can cause dehydration, electrolyte imbalance, kidney failure, circulatory failure, and death.
Burn patients are treated with intravenous fluids to offset dehydration, as well as intravenous nutrients that enable the body to repair tissues and replace lost proteins. Another serious threat to the lives of burn patients is infection. Burned skin is extremely susceptible to bacteria and other pathogens because of the loss of protection by intact layers of skin.
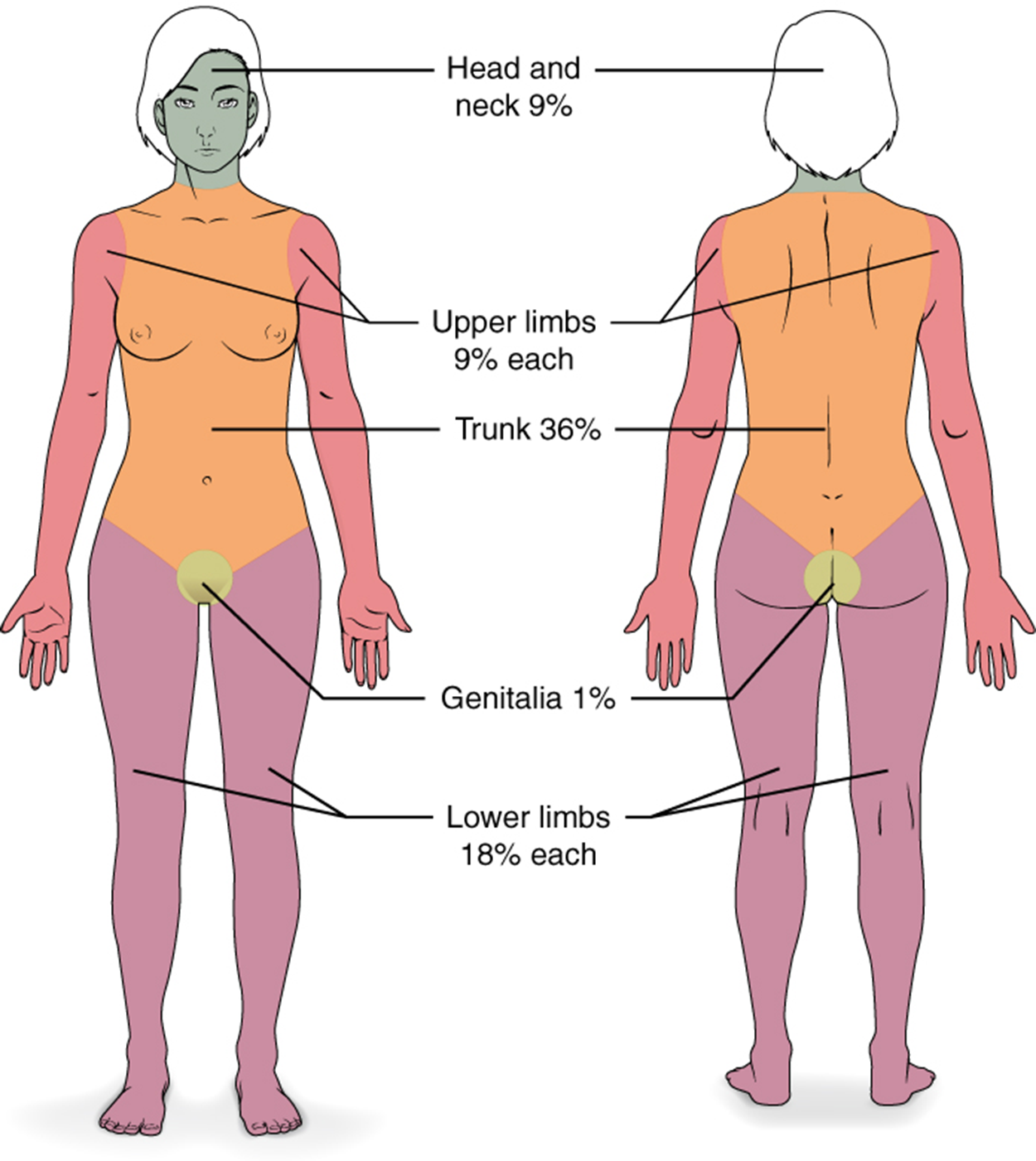
Burns are sometimes measured in terms of the size of the total surface area affected. This is referred to as the “rule of nines,” which associates specific anatomical areas with a percentage that is a factor of nine, as depicted in the image below. In an emergency medical situation, this calculation can help determine how the body is reacting and how to treat the patient (what procedures in what order) to best help the patient. This calculation is also essential for calculating fluid resuscitation, which involves replenishing the fluids that were lost as a result of being burned to restore fluid balance in the body.
IN CONTEXT
The Parkland formula, also known as the Baxter formula, is a widely recognized formula for calculating fluid replacement when burn injury occurs. According to this formula, 2 to 4 ml of Ringer’s lactate solution (a crystalloid fluid solution) should be applied per kilogram of weight per percent of body surface area burned.
Burns are also classified by the degree of their severity.
Most cuts or wounds, with the exception of ones that only scratch the surface (the epidermis), lead to scar formation. A scar is collagen-rich skin formed after the process of wound healing that differs from normal skin. Recall that a scar forms when granulation tissue cannot be formed to fill in the missing tissue. Scar tissue is fibrous in nature and does not allow for the regeneration of accessory structures, such as hair follicles, sweat glands, or sebaceous glands.
Sometimes, there is an overproduction of scar tissue because the process of collagen formation does not stop when the wound is healed; this results in the formation of a raised or hypertrophic (enlarged) scar called a keloid. In contrast, scars that result from acne and chickenpox have a sunken appearance and are called atrophic scars.
Scarring of skin after wound healing is a natural process and does not need to be treated further. Application of mineral oil and lotions may reduce the formation of scar tissue. However, modern cosmetic procedures, such as dermabrasion, laser treatments, and filler injections have been invented as remedies for severe scarring. All of these procedures try to reorganize the structure of the epidermis and underlying collagen tissue to make it look more natural.
Skin and its underlying tissue can be affected by excessive pressure. One example of this is called a bedsore. Bedsores, also called decubitis ulcers, are caused by constant, long-term, unrelieved pressure on certain body parts that are bony, reducing blood flow to the area and leading to necrosis (tissue death). Bedsores are most common in elderly patients who have debilitating conditions that cause them to be immobile. Most hospitals and long-term care facilities have the practice of turning the patients every few hours to prevent the incidence of bedsores. If left untreated by removal of necrotized tissue, bedsores can be fatal if they become infected.
The skin can also be affected by pressure associated with rapid growth. A stretch mark results when the dermis is stretched beyond its limits of elasticity, as the skin stretches to accommodate the excess pressure. Stretch marks usually accompany rapid weight gain during puberty and pregnancy. They initially have a reddish hue but lighten over time. Other than for cosmetic reasons, treatment of stretch marks is not required. They occur most commonly over the hips and abdomen.
When you wear shoes that do not fit well and are a constant source of abrasion on your toes, you tend to form a callus at the point of contact. A callus is a thickened region of skin, formed to protect the underlying tissue from damage. The basal cells of the epidermis are triggered to increase their division, which increases the number of keratinocytes in that region temporarily. Calluses can also form on your fingers if they are subject to constant mechanical stress, such as long periods of writing, playing string instruments, or video games.
SOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION. LICENSE: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.