Table of Contents |
Effective public health strategies focus on preventing disease before it starts and managing conditions effectively when they do occur. This is achieved through a multitiered approach known as the levels of prevention. These levels—primary prevention, secondary prevention, and tertiary prevention—are foundational in shaping public and community health policies and practices aimed at improving community health outcomes.
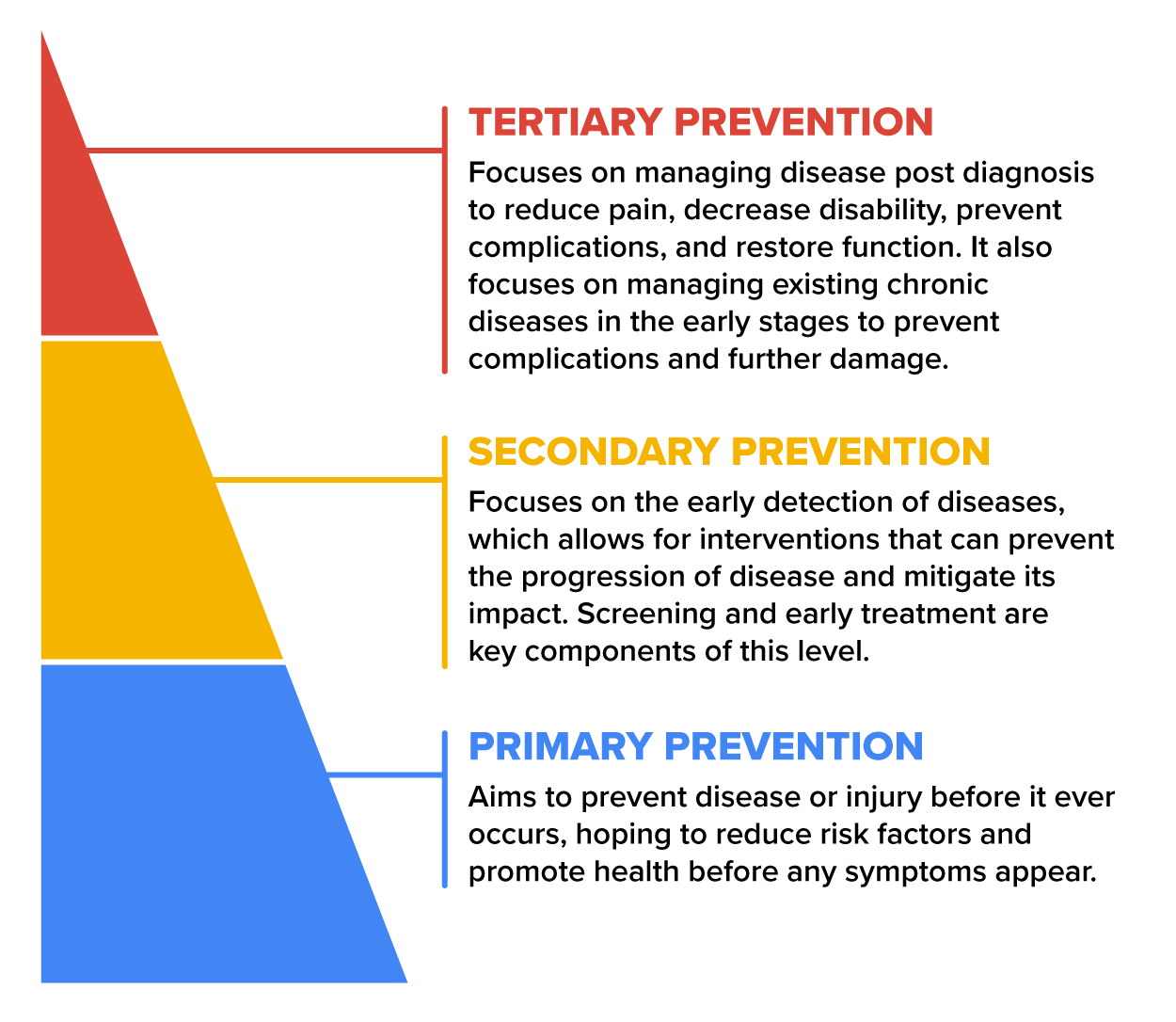
Primary prevention aims to prevent disease or injury before it ever occurs. This is done by preventing exposure to hazards that cause disease or injury, altering unhealthy or unsafe behaviors that can lead to disease or injury, and increasing resistance to disease or injury should exposure occur. Essentially, primary prevention is about reducing risk factors and promoting health before any symptoms appear.
IN CONTEXT
Primary Prevention Practices
Here are a few examples of primary prevention practices in public and community health:
- Vaccination programs: Vaccines are administered to prevent infectious diseases. Polio, once a disease feared globally, has been almost eradicated thanks to effective vaccination campaigns.
- Community water fluoridation: By adjusting the fluoride concentration in municipal water supplies, communities can prevent tooth decay on a large scale.
- Educational campaigns on nutrition and physical activity: Organizations like the American Heart Association offer resources and guidelines to encourage healthy eating and regular physical activity to prevent heart disease and stroke.
Secondary prevention focuses on the early detection of diseases, which allows for interventions that can prevent the progression of diseases and mitigate their impact. Screening and early treatment are key components of this level.
IN CONTEXT
Secondary Prevention Initiatives
Screening programs are critical for diseases such as cancer and diabetes, where early detection significantly affects treatment outcomes. For example, mammography screenings can detect breast cancer early, and blood glucose tests can identify prediabetic conditions before they evolve into full-blown diabetes. Colonoscopies and Pap smears are also secondary prevention measures. Blood pressure checks and cholesterol screenings help identify risk factors for cardiovascular disease and diabetes.
Contact tracing involves identifying and treating the sex partners of someone diagnosed with a sexually transmitted infection to prevent further spread.
Preventive pharmacotherapy, or drug therapy, is the use of medications to prevent diseases from worsening or progressing. For instance, statins may be prescribed to reduce cholesterol levels and prevent cardiovascular diseases.
Tertiary prevention involves managing diseases post diagnosis to reduce pain, decrease disability, prevent complications, and restore function. It focuses on managing existing chronic diseases in the early stages to prevent complications and further damage. This stage involves comprehensive management strategies to maintain the best possible quality of life.
IN CONTEXT
Tertiary Prevention Strategies
- Diabetes management, which involves controlling blood sugar levels, practicing excellent skin care, and exercising to prevent heart disease and blood vessel disorders
- Supportive and rehabilitative services, which provide rehabilitation services for injuries, heart attacks, or strokes to maximize the quality of life
- Prevention of complications in people with disabilities, such as preventing pressure sores in bed-confined individuals (CDC, 2017)
Epidemiologists carefully select relevant data sources, manage existing data, and collect new data when necessary to inform prevention initiatives and protect public and community health. Data management is crucial to the work epidemiologists do, especially in prevention. Epidemiologists working in applied public health have access to various data sources. The sources include notifiable disease case data (primarily, communicable diseases), chronic disease data, injury data, and health risk behavior data. They consider factors such as investigation objectives, scope, data availability, and practicality when selecting relevant data sources for field investigations (Hedberg & Maher, 2018).
Epidemiologists face many data collection challenges. Accessing or collecting clean, valid, reliable, and timely data can be a challenge during field investigations. The new data collected during investigations should meet quality criteria like surveillance data (e.g., quality, definitions, timeliness, completeness, simplicity, generalizability, validity, and reliability). Understanding these terms fully and how they apply to epidemiology are outside the scope of this course. Their overall purpose is to ensure that the data used by epidemiologists are quality data that can safely be used to inform health decisions and recommendations.
Health screenings are essential for maintaining well-being and preventing health problems. They matter because they help in early detection of diseases and health conditions before symptoms appear. Detecting issues early allows for prompt intervention and better outcomes (Office of Disease Prevention and Health Promotion, 2024). Treatment is more effective and easier when problems are caught early. Regular screenings improve the chances of successful management and recovery (Madormo, 2022). Early detection and timely treatment lead to better health outcomes and overall quality of life. Preventive measures can prevent complications.
Screenings also identify risk factors, allowing individuals to make informed decisions about lifestyle changes and preventive actions. Knowing your health status motivates healthier behaviors like exercise, nutrition, and stress management. Health screenings also benefit communities. Regular screenings allow for timely intervention if disease is detected. When individuals receive prompt treatment, it prevents the spread of diseases within communities.
By addressing health issues proactively, communities can reduce the overall burden of illness. Health screenings also raise awareness about prevalent health concerns, where community members can then identify risk factors, symptoms, and available resources to intervene. Lastly, accessible screening, like mobile units for mammography, promotes health equity by ensuring everyone has a chance to detect and manage health conditions. This helps bridge the gaps in health outcomes across diverse populations.

Health screening data empower epidemiologists to inform public health practice regarding health trends, patterns, and risk factors. They use the data to design interventions based on screening results designed for targeted interventions.
EXAMPLE
If a community has high rates of diabetes, they may develop prevention programs or educational campaigns.Epidemiologists advocate for regular screenings to reduce disease severity and complications. They can also help communities with resource allocation to address health issues, policy development, and public health planning.
Disease control strategies in epidemiology include measures to prevent, manage, and mitigate disease impacts. Some key strategies include early detection and reporting of outbreaks and cases, allowing for timely intervention. Surveillance systems play a crucial role in detecting disease clusters and unusual patterns. Recall that isolation and quarantine can reduce the transmission of disease, and contact tracing means identifying individuals who may have been exposed so they can be confirmed as a new case and isolated to prevent the further spread of disease.
Vaccination programs and educating the public on hygiene practices, as well as campaigns to promote preventive behaviors, are all control strategies epidemiologists use. Each person and community is responsible for these activities for the collective benefit of all. Personal responsibility means that individuals have a personal responsibility for their own health and well-being. It involves making informed choices about lifestyle behaviors, such as diet, exercise, and avoidance of harmful substances. Personal responsibility recognizes that our decisions impact our health outcomes. Collective responsibility refers to society sharing responsibility for public health. There is an emphasis on health outcomes influenced by social, economic, and environmental factors beyond individual control. This involves making policies, systems, and environments that promote health for everyone.

Personal protective equipment (PPE) refers to specialized gear worn by individuals to minimize exposure to various hazards. Wearing PPE is a personal and collective responsibility to control disease transmission and protect individual and collective health. In the context of public and community health, PPE serves as a barrier between infectious materials like viruses and bacteria and the skin, mouth, nose, or eyes (mucous membranes) of health care workers and other personnel (Food and Drug Administration [FDA], 2020).
EXAMPLE
PPE includes gloves, gowns and aprons, face masks, respirators, goggles, and face shields to protect the mucous membranes of the face, mouth, nose, and eyes.The purpose of PPE in public and community settings is infection control, safety, compliance with regulatory requirements and guidelines, and improved productivity to enhance employee safety and efficiency.
Earlier in this course, you learned about quarantine and isolation as methods to prevent the spread of disease. Quarantine and isolation are public health practices used to stop the spread of infectious diseases by separating those who are sick from those who are not. Quarantine and isolation are both an individual responsibility as well as a collective one.
Recall that quarantine refers to the separation of individuals who may have been exposed to a disease but do not show symptoms. It helps to monitor symptoms and ensures early detection and containment of the disease. Also, recall that isolation involves separating sick individuals with a contagious disease from those who are not sick. It is used to prevent the spread of infectious diseases.

Lifestyle and behavior management plays a key role in controlling and preventing noncommunicable diseases, such as heart disease, stroke, and diabetes. Healthy eating means consuming a balanced diet that helps reduce the risk of dying from heart disease or diabetes.
This would mean including vegetables and fruits that provide essential vitamins, minerals, and antioxidants. Whole grains that are rich in fiber and nutrients support heart health. Lean (less fatty) proteins like poultry, fish, beans, and nuts are important, as is eating low-fat dairy products, which are essential for bone health. Limiting saturated and trans fats found in processed and fried foods, added sugars, and high salt consumption can reduce the risk of heart disease. Avoiding overeating processed meats and sugar-sweetened drinks and making informed dietary choices contribute significantly to overall well-being and disease prevention.
Earlier in this course, an emphasis on the role of vaccines in preventing the spread of diseases like smallpox was highlighted as a pivotal advancement in public health. Vaccinations are a cornerstone of public health, preventing millions of deaths each year by providing immunity against various infectious diseases. Vaccines work by mimicking the disease agent or administering a weakened, inactivated form of the disease agent to the immune system. Our immune system is an internal mechanism that protects our bodies from disease or fights off disease should we contract one. A vaccine provokes a response from the immune system for a particular disease and protects us from the disease without causing it. This “training” helps the immune system recognize and combat the actual disease pathogen if encountered in the future. Immunization (another word for vaccination) is a global success story, saving millions of lives annually.

When enough people in a community are vaccinated (received a vaccine), the spread of diseases slows down or stops. Germs cannot easily travel from person to person, protecting the entire community. Vaccinated individuals act as a shield to prevent outbreaks and safeguard vulnerable populations. This is the concept of community or herd immunity. Essentially, higher vaccination rates are crucial because they contribute to broader community health by preventing outbreaks (U.S. Department of Health and Human Services [HHS], 2021). They contribute to global health security and are vital in the fight against antimicrobial resistance (when bacteria, viruses, fungi, and parasites no longer respond to medicines). The ongoing COVID-19 pandemic highlights the importance of vaccination efforts.
EXAMPLE
According to WHO (2024), widespread measles vaccination resulted in an 80% drop in measles deaths between 2000 and 2017 globally.Much of the historical contribution of vaccines to public health was covered earlier in this course. Vaccines continue to evolve, protecting us from a wide range of diseases. Vaccines have saved lives more than any other medical invention in history. Their development requires time, resources, and global cooperation.
Social and ethical considerations around vaccines include equitable access to all regardless of socioeconomic status, race, or geographic location. Addressing health disparities in vaccine distribution and reaching historically marginalized communities are crucial. Addressing historical mistrust or misinformation through transparent communication about vaccine safety and development is important. Respecting the autonomy of individuals means they should receive clear information about vaccines, potential risks, and benefits so they can make an informed, voluntary choice. People have the right to accept or decline vaccination.
Vaccines protect not only individuals but also communities. Ethical decision-making guides our path toward a healthier public.
Source: THIS TUTORIAL WAS AUTHORED BY SOPHIA LEARNING. PLEASE SEE OUR TERMS OF USE.
Disclaimer: The use of any CDC and United States government materials, including any links to the materials on the CDC or government websites, does not imply endorsement by the CDC or the United States government of us, our company, product, facility, service, or enterprise.
REFERENCES
Centers for Disease Control and Prevention. (2017, April 6). Picture of America. U.S. Department of Health and Human Services. www.cdc.gov/pictureofamerica/index.html
Food and Drug Administration. (2020). Personal protective equipment for infection control. www.fda.gov/medical-devices/general-hospital-devices-and-supplies/personal-protective-equipment-infection-control
Hedberg, K., & Maher, J. (2018, December 13). The CDC field epidemiology manual: Collecting data. Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. www.cdc.gov/eis/field-epi-manual/chapters/collecting-data.html
Madormo, C. (2022, October 18). The importance of health screenings as you age. Verywell Health. www.verywellhealth.com/health-screenings-with-age-6735854
Office of Disease Prevention and Health Promotion. (2024, May 15). Get screened. U.S. Department of Health and Human Services. health.gov/myhealthfinder/doctor-visits/screening-tests/get-screened
U.S. Department of Health and Human Services. (2021, April 29). Vaccines protect your community. www.hhs.gov/immunization/basics/work/protection/index.html
World Health Organization. (2024). A brief history of vaccines. www.who.int/news-room/spotlight/history-of-vaccination/a-brief-history-of-vaccination