Table of Contents |
Abdominal ultrasound and other types of imaging can be used to detect digestive system disorders. For example, cholecystitis is diagnosed with blood tests and an abdominal ultrasound. Diverticulitis is diagnosed with a CT scan, which can identify inflamed or infected pouches. In addition to blood tests that evaluate liver function and biopsies, liver ultrasounds and CT scans are used to diagnose cirrhosis of the liver.
The U.S. Preventive Services Task Force recommends that adults aged 45 to 75 be screened for colorectal cancer. Several stool-based tests can be used to screen for polyps or colorectal cancer:
- Fecal occult blood test (FOBT) or (gFOBT): Uses a chemical called guaiac to detect blood in the stool. For this test, the patient receives a test kit from their health care provider. At home, they use a small stick or brush to obtain a small amount of stool and place it on a card. The test kit is returned to a lab, where the stool sample is checked for the presence of blood.
- Fecal immunochemical test: Uses antibodies to detect blood in the stool.
- Stool DNA test: Combines the fecal immunochemical test with a test that detects altered DNA in the stool. For this test, an entire bowel movement is collected and sent to a lab, where it is checked for altered DNA and the presence of blood.
If a stool test is positive, then a colonoscopy is scheduled for follow-up testing.
In choosing between FOBT and FIT, there are several considerations. Both can be done at home. Dietary restrictions are typically recommended for FOBT. FIT is considered more accurate, as it is more likely to detect cancer when it is there and less likely to detect other conditions as cancer, when compared with FOBT (Colorectal Cancer Screening, 2020).
The figure below shows a stool specimen container.
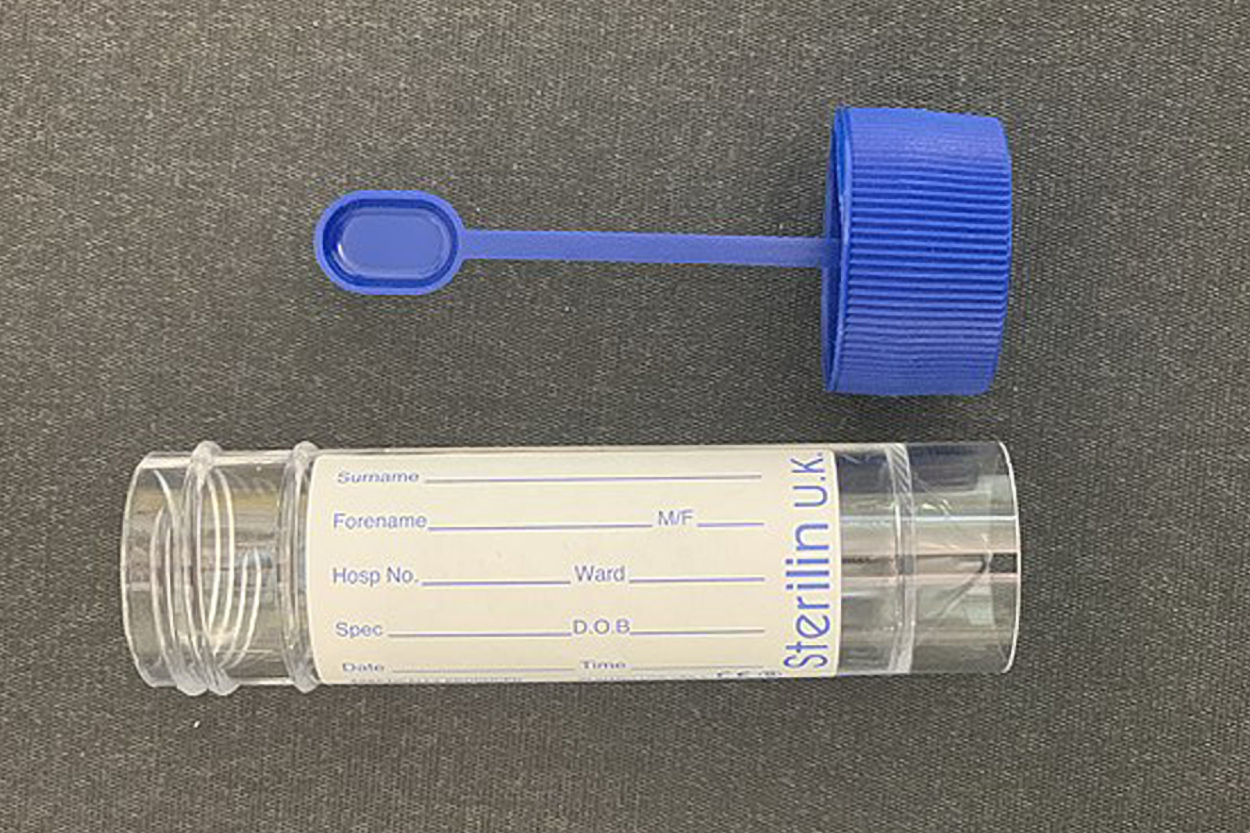 |alt=A clear, labeled container with a cap nearby. The cap has a stick extending to a small oval tip.]]
|alt=A clear, labeled container with a cap nearby. The cap has a stick extending to a small oval tip.]]
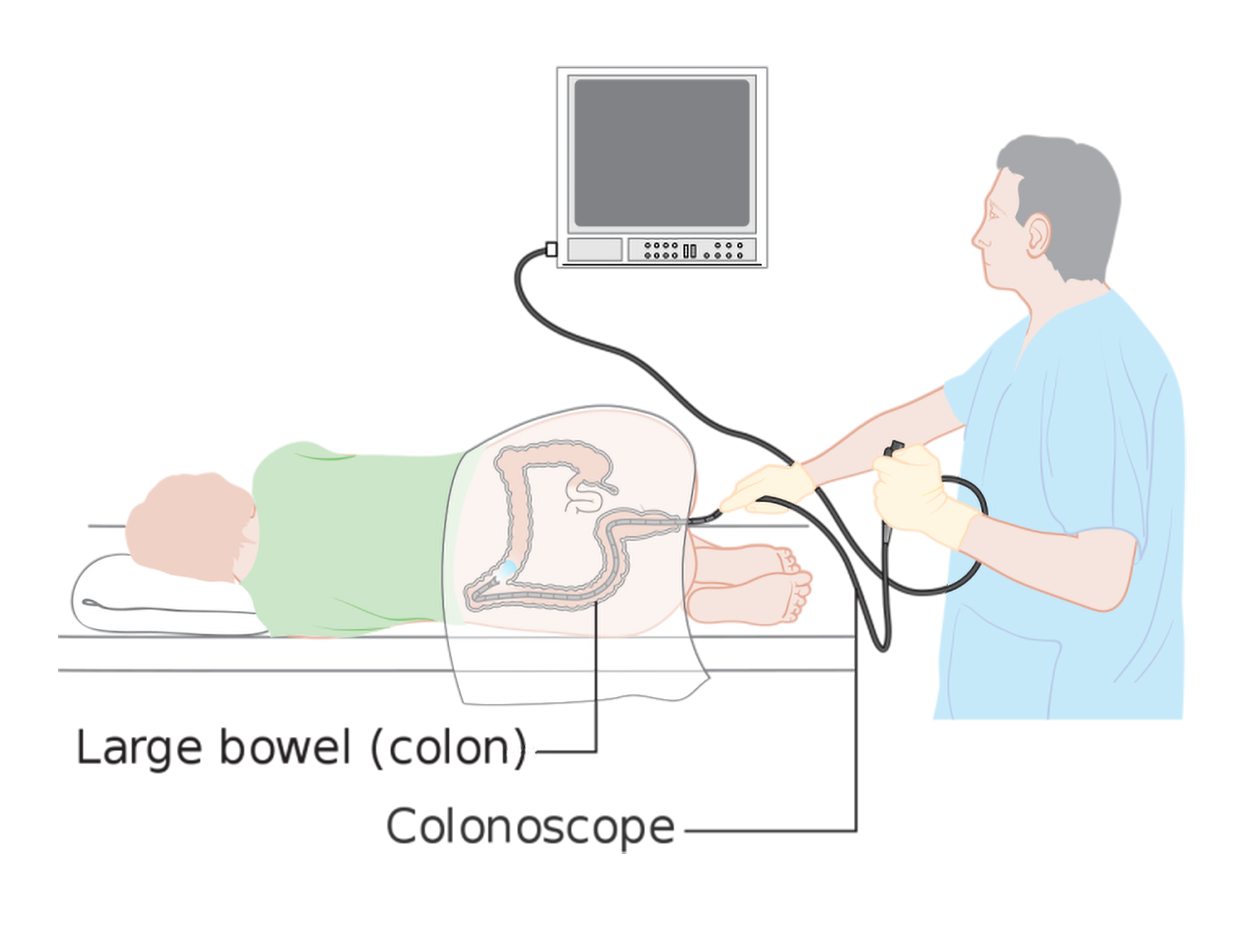
Although the stool-based tests can be useful, people at high risk or who have a positive stool-based test are recommended to have a colonoscopy. A colonoscopy is a procedure that examines the inside of the large intestine, including the colon, rectum, and anus. The colonoscopy has advantages over other testing approaches in that polyps can be removed during the procedure, and it is highly sensitive (UChicago Medicine, n.d.). A sigmoidoscopy is a similar procedure, except that it only examines the sigmoid colon. During both procedures, the physician uses an endoscope, a flexible tube with a lighted camera on the end that is inserted into the anus and colon. Along the way, it sends images of the inside of the large intestine to a screen. This allows the physician to detect abnormalities, such as polyps. The physician can take biopsies during these procedures and can also remove polyps.
The figure below shows a patient undergoing a colonoscopy. The patient lies on their side while the physician inserts a long tube (the endoscope) into the large intestine. An image is shown on a monitor so the doctor can carefully examine the colon walls throughout the procedure.
The American Cancer Society recommends routine colonoscopy screening for colon cancer for individuals of average risk starting at age 45. Colonoscopies are also used to diagnose medical conditions like inflammatory bowel disease or colon cancer.
Colonoscopy prep is very important to the success of the procedure. The health care provider provides detailed instructions to the patient to follow in the days leading up to the procedure. The purpose of these preparations is to make sure the large intestine is as clear as possible for visualization of the tissue. The preparation typically involves a limited diet, with clear liquids before the procedure. Patients need to avoid red liquids as red can be mistaken for blood. In a typical protocol, a strong laxative is taken to purge the bowels on the day before the colonoscopy.
Another option is a virtual colonoscopy (CT colonography), which uses CT scans to create a 3D image of the colon. This procedure has the disadvantage that polyps cannot be removed during the procedure (UChicago Medicine, n.d.).
During an upper GI endoscopy, also called an esophagogastroduodenoscopy (EGD), a doctor uses a flexible tube with a camera to see the lining of the upper gastrointestinal tract, including the esophagus, stomach, and duodenum. During upper GI endoscopy, biopsies may be taken by passing an instrument through the endoscope to take small pieces of tissue from the lining of the esophagus. A pathologist examines the tissue under a microscope.

Upper GI endoscopy, including a biopsy if needed, can be used to diagnose esophageal cancer and GERD, among other conditions.
An upper gastrointestinal series (upper GI series) is an X-ray examination of the upper gastrointestinal (GI) tract. This testing can be used to detect esophageal cancer, among other uses. The esophagus, stomach, and duodenum are made visible on X-ray film by a liquid suspension that may be barium or a water-soluble contrast. If only the pharynx and esophagus are examined with barium, the procedure is called a barium swallow. Barium is a chalky material that appears white on X-ray and coats the inner walls of the digestive tract when administered. Fluoroscopy is often used during an upper GI series to allow the radiologist to visualize the movement of the barium through the esophagus, stomach, and duodenum as a person drinks. After the procedure, if barium is not completely eliminated from the body, constipation and fecal impaction can occur.
The figure below shows an image of an upper GI series that shows a hernia and an obstruction. The barium causes the stomach and esophagus to appear white. Narrowing represents the obstruction.

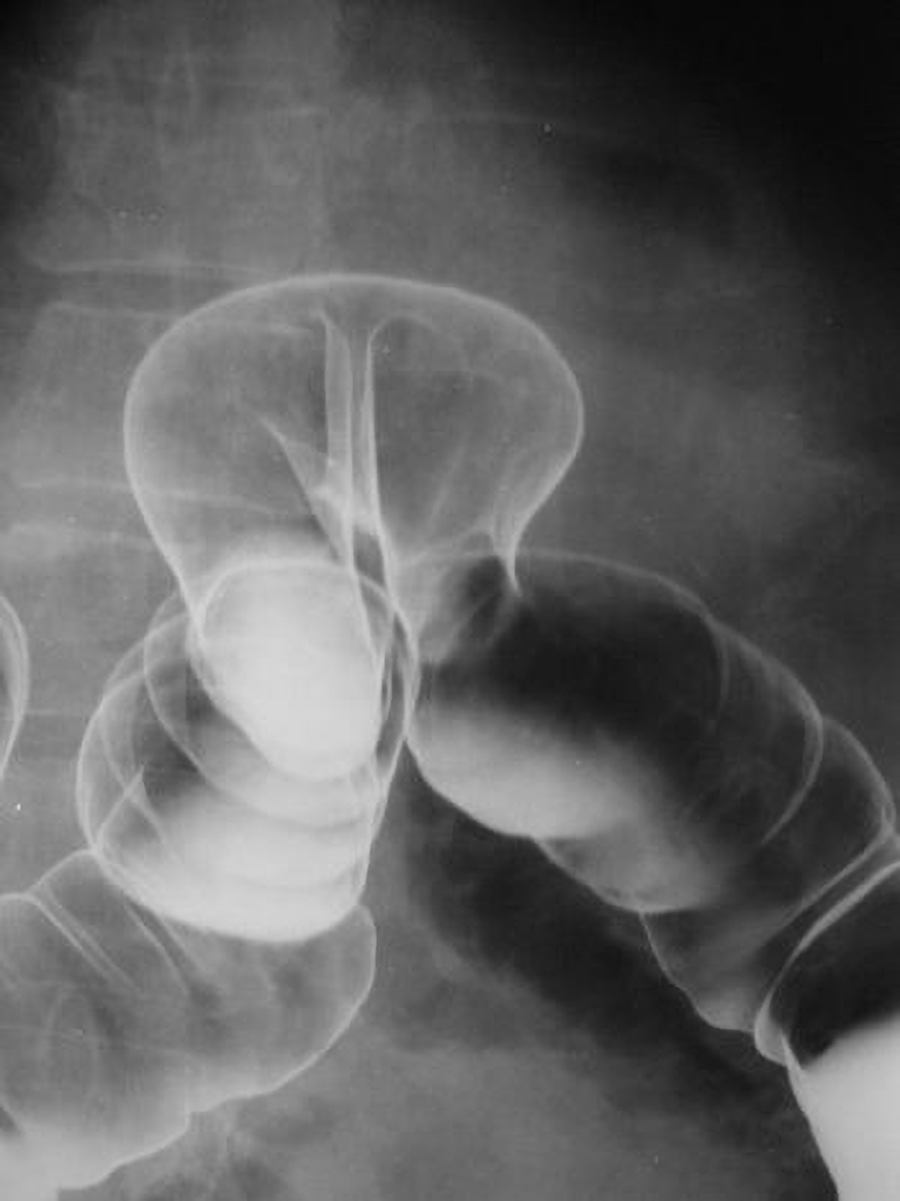
Another diagnostic procedure that uses barium is a barium enema, which is a diagnostic procedure involving the use of a contrast material known as barium. Barium coats the inner wall of the large intestine for visualization. During the procedure, barium is administered into the rectum, along with air (which appears black on X-ray). Fluoroscopy is often used during a barium enema. During fluoroscopy, a continuous X-ray is passed through the large intestine and is transmitted to a monitor so the movement of the barium through the large intestine can be visualized as it is instilled through the rectum. After the procedure, if the barium isn’t completely eliminated from the body, constipation or fecal impaction may occur.
The image below shows a barium enema showing herniation of the colon. The colon bends upward and back down at the site of the herniation. The barium causes the colon to appear white on the left side of the image, on one side of the herniation, and air in the colon causes it to appear black on the right side of the image, on the other side of the herniation.
Some conditions have relatively straightforward treatments.
EXAMPLE
Mild diverticulitis can be treated with rest, diet changes, and antibiotics. Severe or recurring diverticulitis may require bowel resection surgery. Cirrhosis of the liver is treated by treating the cause of the cirrhosis, including treating infections and abstaining from alcohol.Direct-acting antiviral medications (DAAs) have revolutionized treatment for hepatitis C, a viral infection that used to be chronic and which can cause severe complications, including cirrhosis and liver cancer. With DAA treatment that targets the viral life cycle, hepatitis C can be cured with as little as 12 weeks of treatment (Basit et al., 2023).
To remove gallstones in patients with cholecystitis, a procedure called an endoscopic retrograde cholangiopancreatography (ERCP) may be performed that combines an upper endoscopy with X-ray technology. The doctor visualizes the biliary system and then removes gallstones during an endoscopy to relieve immediate symptoms. Cholecystectomy refers to surgery to remove the gallbladder to prevent repeat episodes of gallbladder inflammation, typically performed with a laparoscope, which is a tubular instrument with a light and a camera at the end that is used to view the abdominal or pelvic cavities.
Crohn’s disease and ulcerative colitis are treated with medications, bowel rest, and surgery. No single treatment works for everyone with Crohn’s disease. The goals of treatment are to decrease the inflammation in the intestines and prevent flare-ups of symptoms. Surgery may include small bowel resection or large bowel resection, where part of the small intestine or large intestine, respectively, is removed. In severe cases, proctocolectomy is performed, where the entire colon and rectum are removed. In some cases, an ileostomy is created, where part of the ileum is brought through an artificial opening in the abdomen called a stoma (a stoma is a general term for an artificial opening made into a hollow organ, especially one on the surface of the body leading to the gut or trachea). A removable external collection pouch, called an ostomy appliance, connects to the stoma and collects stool instead of it passing through the anus.
Colon cancer can be treated in several ways. Depending on the severity, there are different types of surgeries that may be performed:
- Polypectomy: Removal of polyps (which may prevent progression to cancer)
- Partial colectomy, also called colon resection surgery: The section of the colon containing the tumor is removed, and healthy colon sections are reattached in a procedure called anastomosis (a general term for joining parts like this; Merriam-Webster, n.d.).
- Colon resection with colostomy: The section of the colon that contains the tumor is removed, but healthy colon sections cannot be reattached, so a colostomy is performed. In a colostomy, the colon is attached to an opening in the abdominal wall called a stoma. Instead of eliminating feces through the anus, it is collected in an external bag.
- Radiofrequency ablation: Heat is used during a procedure to destroy cancer cells.
In addition to surgery, additional medical treatment may be required, such as chemotherapy or targeted therapy (treatment that targets the genes, proteins, and tissues that help colon cancer cells grow and multiply).
Other types of cancer also may require surgery. Early-stage esophageal cancer is most commonly treated with an esophagectomy. This involves removing some or most of the esophagus and creating a new esophagus by pulling up part of the stomach into the chest and neck. Chemotherapy, radiation, targeted therapy, and immunotherapy are also commonly prescribed treatments.
Liver transplantation, in which a donor liver is transplanted into a recipient, is also an option for some conditions. Transplantation is sometimes used for liver cancers, hilar cholangiocarcinoma (a cancer of the bile duct), and cancers that have spread to the liver (a common site of metastasis; Dasari et al., 2025; Mahmud, 2020). Transplantation is also sometimes used to treat other causes of severe liver disease, including end-stage chronic liver disease (Mahmud, 2020).
IN CONTEXT
Weight Loss Treatments
There are many other procedures related to the digestive system, such as bariatric surgery (surgery performed to aid in weight loss). Bariatric surgery includes procedures that reduce the amount of nutrition absorbed from food, so people who have this type of surgery have to be careful with their nutrition and take appropriate supplements (Cleveland Clinic, 2022; Mayo Clinic 2022a). For example, one type of bariatric surgery is the gastric sleeve (sleeve gastrectomy), in which about 80% of the stomach is removed, meaning that someone can only eat a small amount of food at a time (Mayo Clinic, 2024). Another type of bariatric surgery is gastric bypass (roux-en-Y), in which a small pouch of the stomach is connected to the small intestine (Mayo Clinic, 2022b).
Recently, there has been considerable interest in medications called GLP-1 inhibitors or GLP-1 agonists. These medications were first developed to help people with diabetes stabilize their blood sugar, but some are now approved to treat obesity as they have a variety of effects that reduce how much people eat and lead to weight loss and related health improvements (Cleveland Clinic, 2023). There is interest in other possible benefits of these medications, such as their potential to help people with addictive disorders; research is underway into these possibilities (Klausen et al., 2022). However, like all medications, GLP-1 inhibitors have potential adverse effects, and people taking them must be aware of these and make sure to continue to pay attention to maintaining a healthy diet and exercise regimen (Cleveland Clinic, 2023).
Source: THIS TUTORIAL HAS BEEN ADAPTED FROM “OPEN RN | MEDICAL TERMINOLOGY – 2e” BY ERNSTMEYER & CHRISTMAN AT OPEN RESOURCES FOR NURSING (Open RN). ACCESS FOR FREE AT https://wtcs.pressbooks.pub/medterm/ LICENSING: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.
REFERENCES
Colorectal Cancer Screening: ACP Guidance Statements. (2020). American Family Physician, 102(4):250-252. Colorectal Cancer Screening: ACP Guidance Statements | AAFP
Basit H, Tyagi I, Koirala J. Hepatitis C. [Updated 2023 Mar 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK430897/
Colonoscopy, Virtual Colonoscopy, or Stool Test: Which Colon Cancer Screening is Right for Me? (n.d.). UChicago Medicine. Colonoscopy, virtual colonoscopy or stool test: Which colon cancer screening is right for me? - UChicago Medicine
Final Recommendation Statement. Colorectal Cancer Screening. (2021, May 18). United States Preventive Services Task Force (USPSTF). Recommendation: Colorectal Cancer: Screening | United States Preventive Services Taskforce
Terruzzi, V., Paggi, S., Amato, A., & Radaelli, F. (2012). Unsedated colonoscopy: A neverending story. National Library of Medicine doi.org/10.4253/wjge.v4.i4.137
Veldhuijzen, G., Klaassen, N. J. M., Van Wezel, R. J. A., Drenth, J. P. H., & Van Esch, A. A. (2020). Virtual reality distraction for patients to relieve pain and discomfort during colonoscopy. Endoscopy international open, 8(7), E959–E966. doi.org/10.1055/a-1178-9289
Snyder. M., M. Guthrie, & S. Cagle. (2018, July 1). Acute Appendicitis: Efficient Diagnosis and Management. American family physician, 98(1): 25-33.
Farooq, A., Rouleau-Fournier, F., & Brown, C. (2021). Antibiotics alone in the treatment of appendicitis. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 193(21), E769. doi.org/10.1503/cmaj.202777
Dasari, B. V. M., Line, P. D., Sapisochin, G., Hibi, T., Bhangui, P., Hblazun, K. J., Shetty, S., Shah, T., Magyar, C. T. J., Donnelly, C., & Chatterjee, D. (2025). Liver transplantation as a treatment for cancer: comprehensive review. BJS open, 9(3), zraf034. doi.org/10.1093/bjsopen/zraf034
Mahmud N. (2020). Selection for Liver Transplantation: Indications and Evaluation. Current hepatology reports, 19(3), 203–212. doi.org/10.1007/s11901-020-00527-9
Bariatric Surgery (2022, June 9). Cleveland Clinic. Bariatric (Weight Loss) Surgery: Types & Requirements
Should I Take Vitamins and Supplements After Weight-Loss Surgery? (2022a, April 8). Mayo Clinic Health System. Vitamins after bariatric surgery - Mayo Clinic Health System
Sleeve Gastrectomy. (2024, August 2). Mayo Clinic. Sleeve gastrectomy - Mayo Clinic
Gastric Bypass (Roux-en-Y). (2022b, June 25). Mayo Clinic. Gastric bypass (Roux-en-Y) - Mayo Clinic
Klausen, M. K., Thomsen, M., Wortwein, G., & Fink-Jensen, A. (2022). The role of glucagon-like peptide 1 (GLP-1) in addictive disorders. British Journal of Pharmacology, 179(4), 625–641. doi.org/10.1111/bph.15677
Merriam-Webster. (n.d.). Anastomosis. In Merriam-Webster.com dictionary. Retrieved July 22, 2025, from www.merriam-webster.com/dictionary/anastomosis