Table of Contents |
There are several standard laboratory tests that are commonly run in medical clinics.
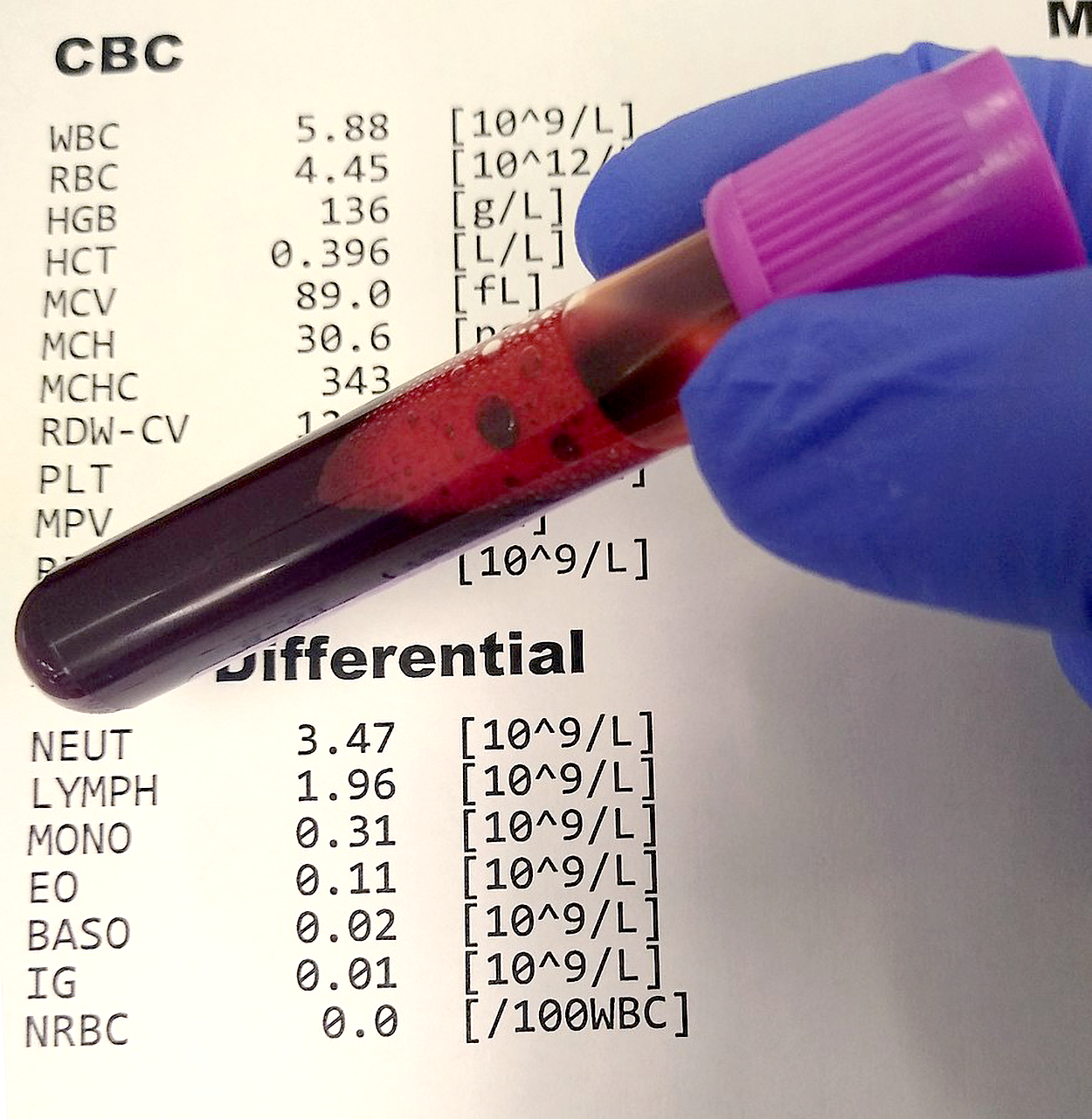
A complete blood count (CBC) is a blood test performed in a laboratory that provides a comprehensive assessment of various blood components, including RBCs, WBCs, platelets, hematocrit (HCT), and hemoglobin (Hgb). These parameters help evaluate the overall health of the hematological system and can indicate anemia, infection, or other blood disorders. A CBC with differential includes an additional measurement of the different types of white blood cells (i.e., neutrophils, lymphocytes, monocytes, eosinophils, and basophils).
The figure below shows an illustration of CBC with differential test results indicated behind a tube of drawn blood.
The table below shows some medical terms related to components of a CBC.
| Term | Abbreviation | Example of relevant conditions |
|---|---|---|
| Red blood cell count | RBC |
Erythrocytosis (elevated) Anemia (too low) |
| White blood cell count | WBC |
Leukocytosis (elevated) Leukopenia (too low) |
| Platelet count | PLT |
Thrombocytosis (elevated) Thrombocytopenia (too low) |
| Hematocrit | Hct |
Polycythemia (too many RBCs) Hypoxia (insufficient oxygen) |
| Hemoglobin | Hgb |
Polycythemia (too many RBCs) Hypoxia (too little oxygen) |
Other terms you may encounter include:
Other common tests examine metabolic processes. These include a basic metabolic panel (BMP) and a comprehensive metabolic panel (CMP).
The BMP includes measurements of electrolytes (sodium, potassium chloride, and bicarbonate). It also measures creatinine and blood urea nitrogen (BUN), which gives information about kidney function (Cleveland Clinic, 2024). The CMP includes additional tests, including tests that give information about liver function: alanine transaminase (ALT), aspartate transaminase (AST), bilirubin, and albumin (Cleveland Clinic, 2024).
It is often important to know whether someone’s blood is clotting normally. This can help in identifying clotting disorders and can be important to monitor someone taking blood-thinning medication (anticoagulants). Monitoring is especially important for people taking heparin, and especially warfarin, but newer anticoagulants, called direct oral anticoagulants (DOACs) do not require the same type of monitoring (McRae et al., 2021).
Examples of these tests include:
- Prothrombin time (PT)
- International normalized ratio (INR)
- Partial thromboplastin time (PTT)
- D-dimer test
A variety of tests can be used to measure inflammation, immune function (e.g., to identify autoimmune disease), and infections.
C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are both used to detect inflammation and autoimmune disease. The antinuclear antibody (ANA) test is used to detect antinuclear (ANA) antibodies because elevated levels of these antibodies suggest autoimmune diseases such as lupus.
Blood cultures can be used to identify which pathogen is causing an infection and to determine its susceptibility to different treatments. Bacteremia (a bacterial infection in the blood) and sepsis. Sepsis is a life-threatening condition that arises when the body’s response to an infection causes injury to its own tissues and organs. Sepsis can lead to significant health complications or death, especially if not recognized early and treated promptly. It often presents with fever, increased heart rate, increased breathing rate, and confusion.
Serologic (blood tests) can be used to identify particular pathogens. For example, a hepatitis panel tests for three types of hepatitis (A, B, and C), an HIV test detects the human immunodeficiency virus (HIV), and the Monospot test detects the Epstein-Barr virus, which causes mononucleosis (Quest Diagnostics, n.d.).
Some specialized tests are used to test hormone levels or detect cancer. Tests of hormone levels are available for cortisol, insulin, testosterone, estrogen, and other hormones. Thyroid hormones are tested to detect hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid). Thyroid tests include TSH (thyroid-stimulating hormone, which stimulates the thyroid gland) and two hormones produced by the thyroid: T3 and T4.
Tumor markers that can be tested include the PSA, CA-125, and CEA tests. PSA (prostate-specific antigen) is used to detect prostate cancer. PSA testing is used in routine screening. CA-125 (cancer antigen 125) can be used to detect cancer recurrence, to assess a particular cancer treatment, and sometimes for ovarian cancer detection in patients with particularly high risk, as it is not helpful for patients at lower risk, as so many other conditions can raise CA-125 levels (Mayo Clinic, 2025). The CEA (carcinoembryonic antigen) test is useful for monitoring cancer treatment and detecting recurrence of certain cancers (Cleveland Clinic, 2025).
In traditional blood donation, a unit of whole blood is taken from a donor and sent to a laboratory, where it is separated into its four components: red blood cells, white blood cells, platelets, and plasma. The components are stored and administered to patients who need blood products transfused after surgery, after a severe injury/trauma, or to treat a severe disease or hematological condition. In contrast, during apheresis, a specific component is removed from a donor’s blood, and the remaining components are returned to the donor while they are still connected to the machine.
Donor apheresis takes longer than a whole blood donation, but it is easy and painless and has many benefits.
EXAMPLE
An apheresis double red-cell donation (called erythropheresis) separates red blood cells and returns the remaining “non-targeted” plasma and platelets to the volunteer donor. This allows for the collection of twice as many red blood cells from one donation as they would in a whole-blood donation. As another example, a platelet apheresis donation can provide as many platelets as those obtained in four to six whole-blood donations.The figure below shows an erythropheresis machine, which is a device with attached bags of blood and test tubes of blood nearby.

Plasmapharesis is used to separate plasma from other blood components. This can be used to obtain plasma for use in other patients, or to remove plasma that contains harmful antibodies or other substances. Plasmapheresis is used to treat conditions such as myasthenia gravis and Guillan-Barré syndrome (an autoimmune condition; Cleveland Clinic, 2022).
A blood product is any therapeutic substance derived from human blood. Types of blood products include whole blood, packed red blood cells (pRBCs), individual factor concentrates, fresh frozen plasma (FFP), platelet concentrates, and cryoprecipitate (i.e., plasma rich in proteins). Packed red blood cells contain RBCs, but not serum (UTMB Health, n.d.). Transfusion of blood products is a common procedure, with nearly 16 million blood components transfused each year in the United States. Nurses typically provide blood transfusions after they are prescribed by a healthcare provider.
In severe cases of symptomatic, severe anemia (i.e., dyspnea or chest pain) or hemoglobin levels less than 7 g/dL, transfusions of red blood cells are prescribed to rapidly increase hemoglobin levels.
The figure below shows a hanging bag of blood labeled clearly as blood type B. The blood type (i.e., A, B, AB, or O) and the Rh factor positive or negative) are indicated on the label to compare with the patient’s lab results. Health care agencies have strict safety procedures that nurses and other health care personnel follow when providing a blood transfusion to prevent the administration of incompatible blood to a patient.
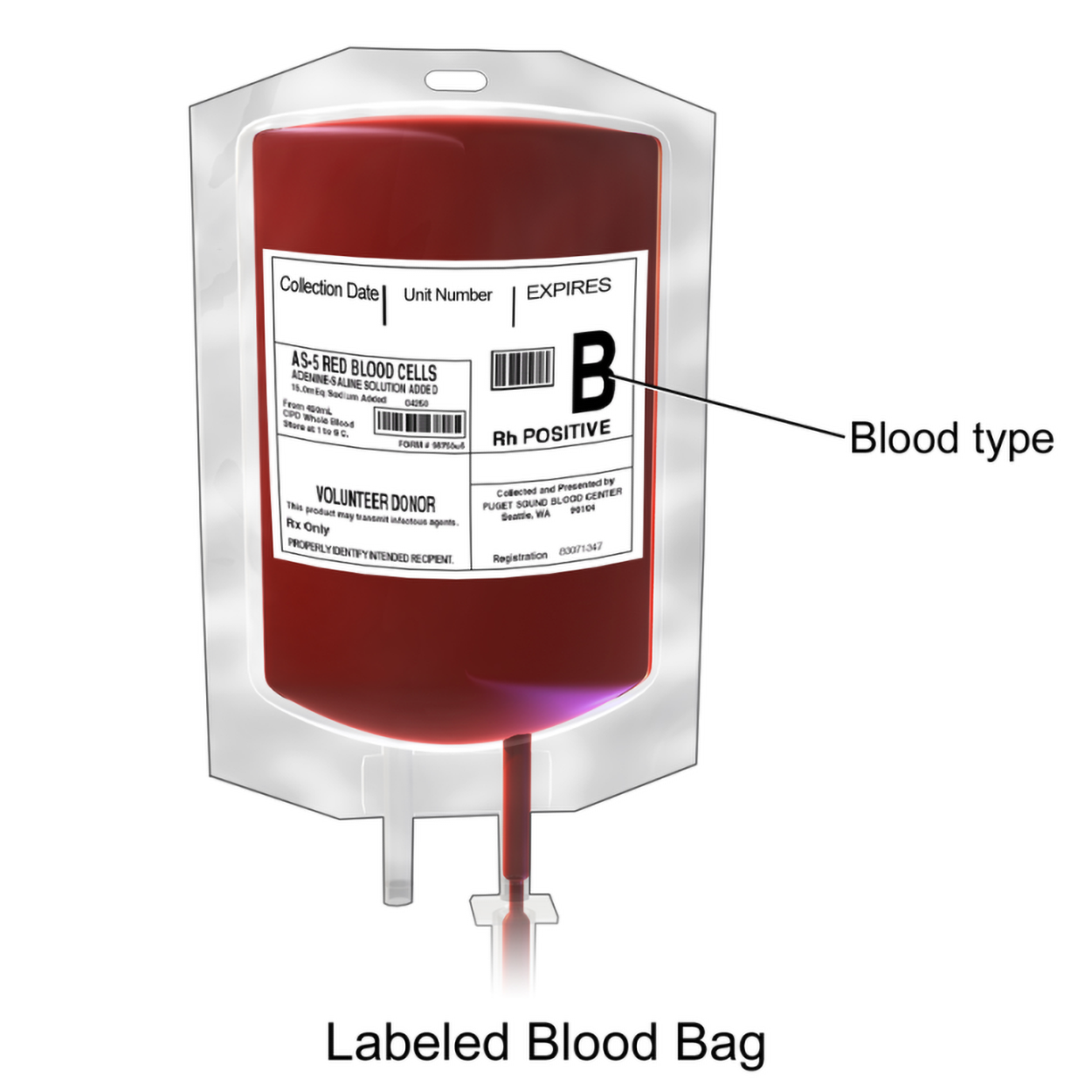
When performing blood transfusions, it is essential to make sure that the blood is compatible. Remember that the ABO blood groups and Rh factor must be considered. Crossmatching is performed before transfusions to check for any incompatibilities. Most importantly, the patient’s red blood cells are exposed to serum from the donor (in other words, the fluid of plasma with no clotting factors). The patient’s serum and cells from the donor can also be mixed to check for a reaction (WebMD, 2025). This helps to ensure that there will be no compatibility issues from the transfusion. If a patient receives incompatible blood, a hemolytic reaction occurs. Remember that hem/o is blood, and –lysis means splitting or dissolution. In a hemolytic reaction following a blood transfusion, the patient’s immune system targets the donor’s red blood cells and destroys them. If there is a serious mismatch (like giving a patient with type A blood a transfusion from a donor with type B blood), then the result is a potentially dangerous reaction. Similar approaches are required for safe organ transplantation.
Bone marrow aspiration involves the extraction of a small sample of liquid bone marrow from the center of a patient’s bone. Common sites for bone marrow aspiration include the pelvic bone and sternum. The procedure is typically performed after local anesthesia is administered, and then the provider inserts a needle into the bone marrow space and draws out a liquid sample. The aspiration allows for laboratory analysis of the cellular components of the bone marrow (i.e., red blood cells, white blood cells, and platelets). Bone marrow aspiration is helpful for determining the presence of severe blood disorders, such as leukemia, and is also used to monitor disease progression or treatment effectiveness.
Bone marrow biopsy involves obtaining a small core of bone and marrow tissue from the bone marrow space. The procedure is often performed in conjunction with bone marrow aspiration.
The figure below shows a bone marrow biopsy. A needle is used to take a sample from the hip. A close-up shows that the needle needs to go through the bone to the bone marrow inside.
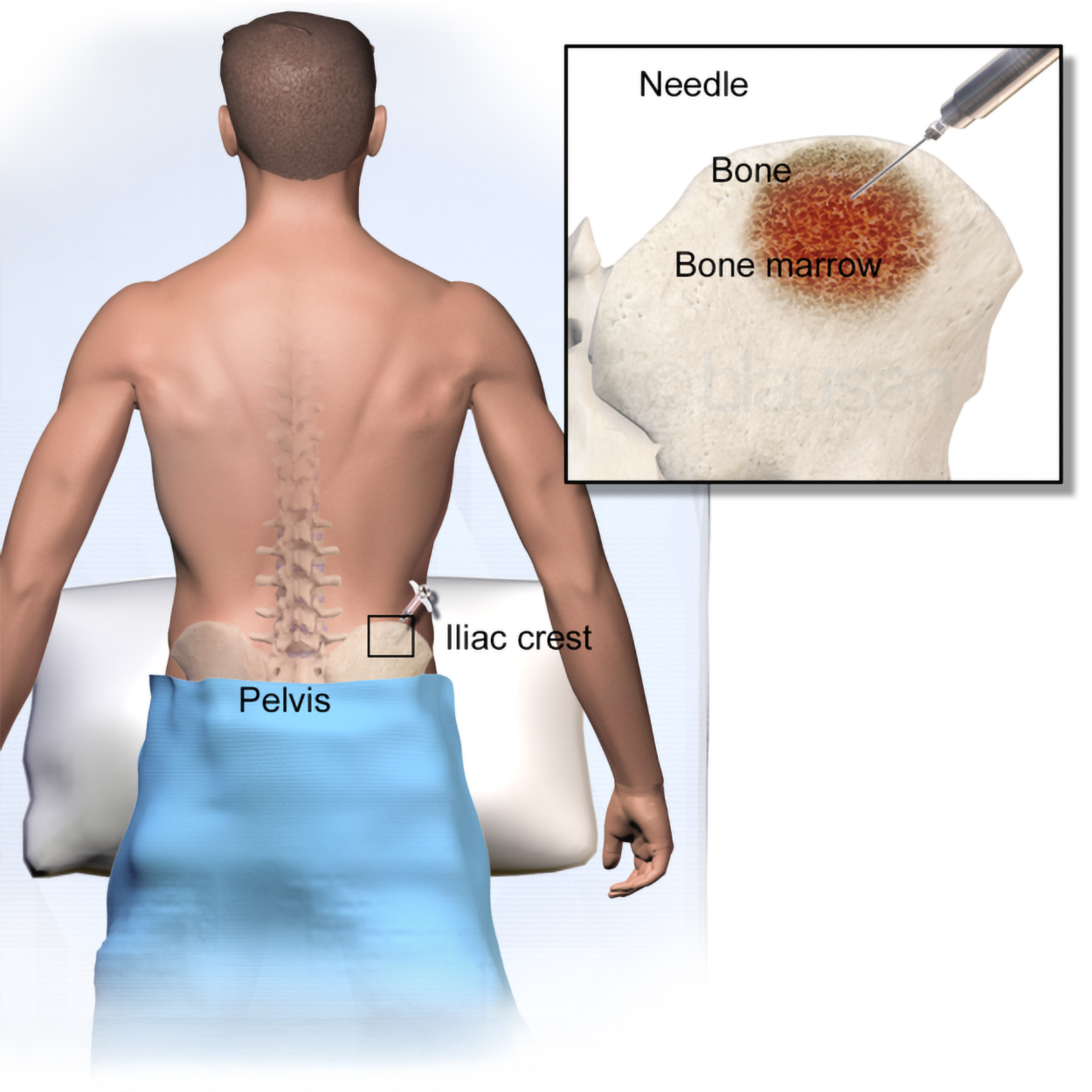
In bone biopsy, in contrast to the bone marrow aspiration procedure, the provider uses a larger needle during bone marrow biopsy to remove a cylindrical section of both the bone and marrow. Bone marrow biopsy provides a comprehensive evaluation of the bone marrow, allowing for a closer assessment of the bone marrow’s cellular density, structure, and the presence of any abnormal or diseased cells. It helps diagnose a wider range of conditions, including non-hematological disorders like metastatic cancers and immune diseases that may infiltrate the bone marrow.
Another approach to examine bone marrow is bone marrow MRI. This technique can be used to examine bone marrow features such as the proportions of red and yellow bone marrow, characteristics of lesions, and changes over time (Vilanova et al., 2024).
Bone marrow transplant, also called stem cell transplant, is a potentially curative treatment for severe hematological diseases like sickle cell disease, as well as cancer like leukemia. It typically involves the administration of chemotherapy to destroy the patient’s existing bone marrow and then replacing the bone marrow with healthy stem cells donated from a compatible donor. If successful, transplantation can be curative and result in the patient’s bone marrow taking over the production of healthy red blood cells, white blood cells, and platelets. However, patients undergoing this procedure with donated stem cells must take immunosuppressive medication for the remainder of their lives.
Immunotherapy harnesses the immune system for some purpose. For example, one type of immunotherapy uses a specific type of antibodies developed in the lab to target cancer cells for the immune system to attack. There are also vaccines to teach the immune system to respond to cancer cells and medications that affect immune system function (National Cancer Institute, 2019).
Immunodeficiencies are sometimes treated using intravenous immunoglobulin G (IVIg). This provides antibodies (immunoglobulins) that supplement the body’s own responses. This can be used for a variety of disorders, including HIV and lupus (Cleveland Clinic, 2024). As you learned in Immune System and Immune Response, immunoglobulins can also be used for other purposes, such as prophylactic treatment following rabies exposure (CDC, 2024).
Because the lymphatic system plays such an important role in the immune response and white blood cell function, there are some procedures to know related to the lymphatic system as well. Pay attention to the word parts to help remember these terms.
Source: THIS TUTORIAL HAS BEEN ADAPTED FROM “OPEN RN | MEDICAL TERMINOLOGY – 2e” BY ERNSTMEYER & CHRISTMAN AT OPEN RESOURCES FOR NURSING (Open RN). ACCESS FOR FREE AT https://wtcs.pressbooks.pub/medterm/ LICENSING: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.
REFERENCES
Basic Metabolic Panel. (2024, October 21). Cleveland Clinic. Basic Metabolic Panel (BMP): What It Is, Procedure & Results
Comprehensive Metabolic Panel. (2024, July 3). Cleveland Clinic. Comprehensive Metabolic Panel (CMP): What It Is & Results
McRae, H. L., Militello, L., & Refaai, M. A. (2021). Updates in anticoagulation therapy monitoring. Biomedicines, 9(3), 262. doi.org/10.3390/biomedicines9030262
Hepatitis Panel, General. (n.d.). Quest Diagnostics. Hepatitis Panel, General | Test Detail | Quest Diagnostics
CEA Test. (2025, June 5). Cleveland Clinic. CEA Test (Carcinoembryonic Antigen): What It Is & Results
CA 125 Test. (2025, March 7). Mayo Clinic. CA 125 test - Mayo Clinic
Plasmapheresis and Plasma Exchange. (2022, September 9). Cleveland Clinic. Plasmapheresis (Plasma Exchange): Therapy, Procedure & What It Is
WebMD Editorial Contributors. (2025, April 28). What is Blood Crossmatching? WebMD. Blood Crossmatching: The First Step in Blood Transfusions
Red Blood Cells. (n.d.). UTMB Health. Red Blood Cells
Vilanova, C., Martín-Noguerol, T., García-Figueiras, R., Baleato-González, S., & Vilanova, J. C. (2024). Bone marrow magnetic resonance imaging (MRI): morphological and functional features from reconversion to infiltration. Quantitative Imaging in Medicine and Surgery, 14(11), 7969–7982. doi.org/10.21037/qims-23-1678
Immunotherapy to Treat Cancer. (2019, September 24). National Cancer Institute. Immunotherapy for Cancer - NCI
IVIG (Intravenous Immunoglobulin) (2024, October 10). Cleveland Clinic. IVIG (Intravenous Immunoglobulin): Treatment & Side Effects
Rabies post-Exposure Prophylaxis. (2024, June 20). Centers for Disease Control and Prevention (CDC). Rabies Post-exposure Prophylaxis | Rabies | CDC
Lymphangiography. (2022, May 10). Cleveland Clinic. Lymphangiography: What It Is, Purpose, Procedure & Risks
Lymphscintigraphy. (2023, November 17). Cleveland Clinic. Lymphoscintigraphy: What It Is, Procedure & Side Effects
Lymphadenectomy. (2022, October 15). Cleveland Clinic. Lymphadenectomy: Surgery Definition, Procedure & Types
Sentinel Node Biopsy. (2024, October 31). Mayo Clinic. Sentinel node biopsy - Mayo Clinic