Table of Contents |
The United States healthcare system is known to be complex, excellent, and yet, imperfect. While the U.S. is ranked highly for healthcare innovation and healthcare quality, there is significant room for improvement. The government, as well as groups such as the American Hospital Association, American Medical Association, American Nursing Association, and the National Association for Healthcare Quality, among many others, work to enact policies and increase the quality of healthcare in the U.S. While quality is a focus, some consumers would say that their experience hasn’t been a quality one.
Does this sound like a very difficult task? Indeed, it is a challenge. The better the healthcare manager understands the healthcare system, the more equipped they will be to lead their organization. With this in mind, this tutorial will give you the basics that are important to know as the first step to success as a manager in healthcare.
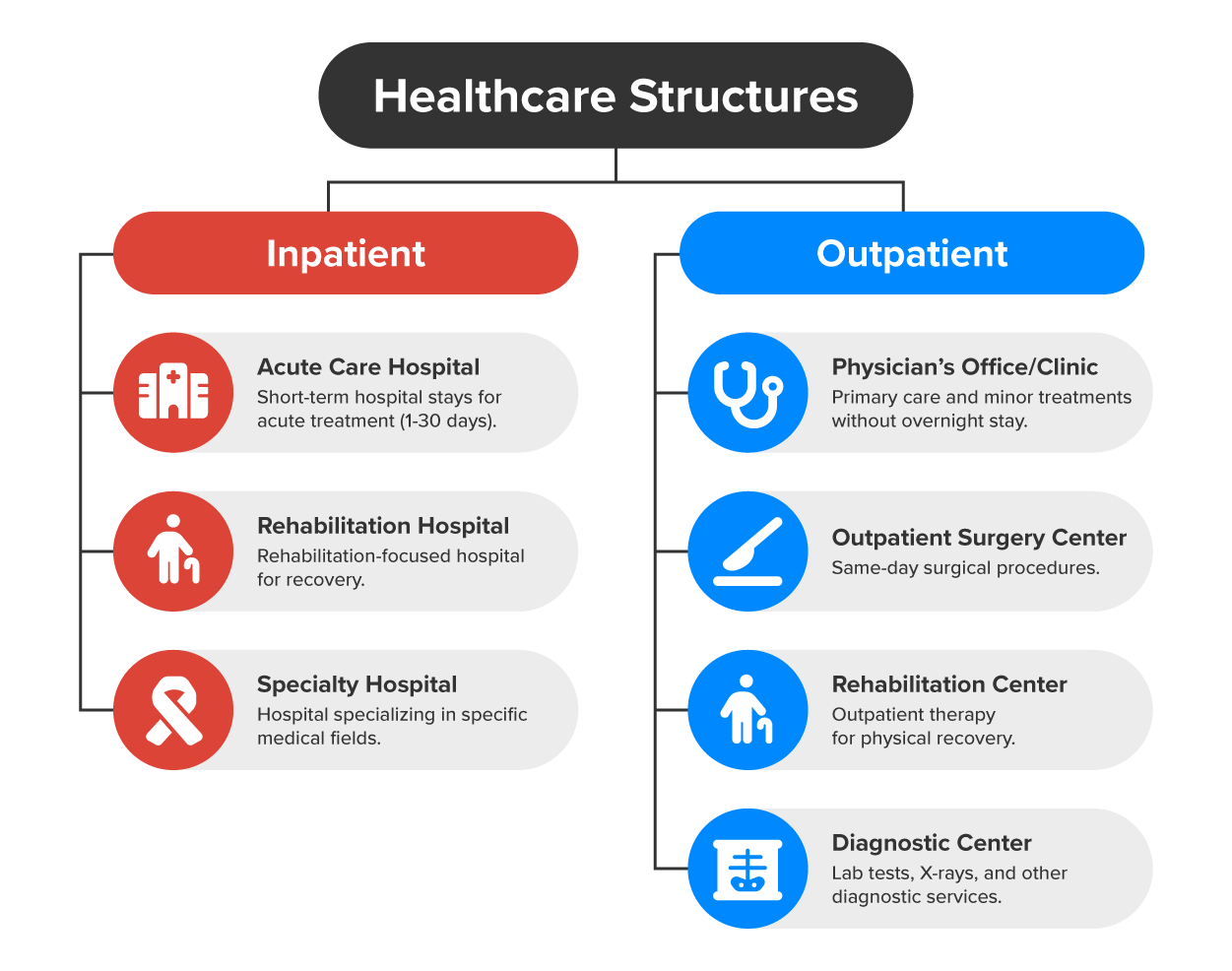
There is a wide variety of healthcare organizations in the United States, each with a specific focus or specialty. Healthcare can be categorized as inpatient (refers to a hospital patient where the patient stays overnight) or outpatient (healthcare that is provided, and the patient returns home the same day). These organizations can range widely in size and type of ownership, but each is important for a person’s continued care.
IN CONTEXT
Inpatient care is typically provided at a hospital. There are different types of hospitals, but most are considered acute care (short-term care usually lasting 1–30 days) hospitals. There are also rehabilitation hospitals and other specialty hospitals. Outpatient care has an even wider variety of healthcare organizations. The most common would be the physician’s office or clinic where patients go for a quick episode of care. Others may include outpatient surgery centers, rehabilitation centers, and diagnostic centers that may specialize in labs, x-rays, and other diagnostic services.
Each healthcare organization must provide the services necessary to meet the mission of the organization.
EXAMPLE
Some healthcare organizations need lab and x-ray services, while others don’t. Some healthcare organizations conduct surgery, while others don’t. These are just a couple of examples to consider how different each organization might be, adding to the complexity of healthcare access and delivery.While each healthcare organization is unique, they are typically more similar in their management and leadership structure. Most are governed by a board of directors who manage the executive-level managers such as the CEO, CIO, and chief of staff. Under the executives will be professional staff, healthcare providers, and department heads. Under department heads are administrative and support staff. Each level has specific responsibilities, a specific pay structure, and specific requirements for education, experience, and credentials or licensure.
Healthcare organizations are highly regulated by governmental entities as well as accreditation and licensing bodies. First, each healthcare organization must be licensed by the state in which it is doing business. Each healthcare organization must also comply with local laws. Federally, organizations must follow regulations related to payment and quality of care. The main regulatory organization is the Centers for Medicare & Medicaid Services (CMS), the federal agency that provides health coverage to more than 160 million through Medicare, Medicaid, the Children's Health Insurance Program, and the Health Insurance Marketplace (About Us, n.d.). Healthcare organizations must comply with the CMS rules if they wish to bill them for Medicare and Medicaid patients.
The second most prominent regulatory body is The Joint Commission (the organization that accredits healthcare organizations based on a set of quality standards and requirements). Almost all hospitals in the U.S. are accredited by The Joint Commission. It is such a rigorous set of standards that if a hospital is accredited by The Joint Commission, it automatically passes the CMS Conditions of Participation (the quality and safety standards that must be met for a healthcare organization to be able to bill for Medicare and Medicaid patients). Both sets of standards ensure that a healthcare organization is performing to the level of these high standards and are meant to assure the healthcare consumer that the organization is a safe and trusted care provider.
The United States is unique since it is one of the only developed countries without a universal health insurance program. This significantly adds to the complexity of the healthcare system. Payment for services may come from government funding, private insurance, and private pay. Within the private insurance category, some employees receive it as a benefit through their workplace, while others can purchase insurance on their own through the healthcare marketplace. Many are fighting for healthcare reform that would make healthcare coverage more affordable and accessible.
Healthcare organizations face significant financial challenges, such as rising operational costs, fluctuating reimbursement rates, and the need to invest in new technologies and infrastructure. Balancing financial sustainability with the provision of high-quality care remains a persistent challenge.
IN CONTEXT
Imagine a hospital CEO is faced with the decision of whether to invest in advanced medical equipment, such as a new MRI machine, which would significantly enhance the hospital's diagnostic capabilities and improve patient outcomes. However, this equipment is expensive, and the hospital is already operating with thin financial margins. On one hand, investing in the MRI machine could attract more patients, improve care quality, and enhance the hospital's reputation. On the other hand, the CEO must consider the hospital’s financial sustainability, especially if patient volume doesn’t increase enough to cover the high upfront costs and maintenance of the equipment. The CEO must balance the need to provide high-quality care with the financial constraints, potentially looking at options like securing grants, exploring partnerships, or adjusting the hospital's budget to find a way to make the investment without jeopardizing overall financial health.
Human resources and staffing in healthcare organizations face a multitude of complex challenges that can significantly impact the quality of care provided to patients. One of the most pressing issues is the persistent shortage of qualified healthcare professionals. Fields such as nursing, radiology, and various specialties often experience significant gaps, making it difficult for organizations to recruit and retain skilled personnel. This shortage can lead to increased workloads for existing staff, contributing to burnout and further exacerbating turnover rates.
IN CONTEXT
High turnover is a critical concern in healthcare settings. The demanding nature of the work, combined with emotional strain and long hours, often leads professionals to seek less stressful opportunities elsewhere. This cycle creates instability within teams, resulting in increased recruitment costs and a potential decline in the quality of patient care as well as morale.
In addition, managing a wide range of staff with significant differences in education level and experience, many different licenses and credentials, and various shifts all add to the complexity of managing the healthcare workforce. Teamwork is a necessity, and not all staff want to be a team player. Conflicts can bring tension and require extensive communication among the team. It is also important to ensure that all staff receive continuing education in an industry where change is the norm.
Health Insurance Portability and Accountability Act (HIPAA) (a U.S. law that protects patient privacy by setting standards for the secure handling of personal health information by healthcare providers, insurers, and related entities) is the most prominent set of regulations in healthcare, but healthcare organizations must spend a significant amount of time ensuring compliance with a variety of laws and regulations. All these legal mandates require staff training and continuous monitoring of policies and procedures to provide patients with healthcare that meets the legal requirements. Most laws focus on patient care, safety, privacy, and security. Other laws and regulations focus on patients' rights and ethics. Many healthcare organizations will have an ethics committee and legal representation to assist with difficult situations and the required decisions.
Patient rights include the right to autonomy (the right of patients to make informed decisions about their care) and informed consent. These are related in that a patient has the right to all information about a procedure or treatment plan that allows them to make an informed consent to treatment. Only then can a patient make an autonomous decision about their care. Other patient rights include the right to treatment, the right to confidentiality, and the right to get a second opinion.
Ethical decision making is closely related to following laws, and sometimes there is a thin line between the two. Common ethical dilemmas in healthcare relate to life and death situations such as abortion and end-of-life care. Other ethical issues might be around organ transplants, resource allocation, patient autonomy, and “do not resuscitate” orders, to name a few.
Healthcare organizations play a critical role in society by ensuring the well-being of individuals and communities. Their value extends beyond the provision of medical services. They are often integral to the social fabric and economy of a neighborhood or entire town, and they provide a connection to quality of life.
Source: THIS TUTORIAL WAS AUTHORED BY SOPHIA LEARNING. PLEASE SEE OUR TERMS OF USE.
REFERENCES
About CMS. CMS.gov. (n.d.-a). www.cms.gov/about-cms
Historical. CMS.gov. (n.d.-b). www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/historical#:~:text=U.S.%20health%20care%20spending%20grew,trillion%20or%20%2413%2C493%20per%20person.