Table of Contents |
The size, shape, and number of erythrocytes (red blood cells, RBCs) and the number of hemoglobin molecules can have a major impact on a person’s health. When the blood is unable to transport enough oxygen to the body because RBC numbers are low or hemoglobin is deficient, the general condition is called anemia.
The effects of the various anemias are widespread because reduced numbers of RBCs or hemoglobin will result in lower levels of oxygen being delivered to body tissues. Because oxygen is required for tissue functioning, anemia produces fatigue, lethargy, and an increased risk of infection. An oxygen deficit in the brain impairs the ability to think clearly and may prompt headaches and irritability. Furthermore, lack of oxygen leaves the patient short of breath, even as the heart and lungs work harder in response to the deficit.
There are more than 400 types of anemia, and more than 3.5 million Americans suffer from this condition. Blood loss anemias (hemorrhagic anemias) are fairly straightforward. In addition to bleeding from wounds or other lesions, these forms of anemia may be due to ulcers, hemorrhoids, inflammation of the stomach (gastritis), and some cancers of the gastrointestinal tract. The excessive use of aspirin or other nonsteroidal anti-inflammatory drugs such as ibuprofen can trigger ulceration and gastritis. Excessive menstruation and loss of blood during childbirth are also potential causes.
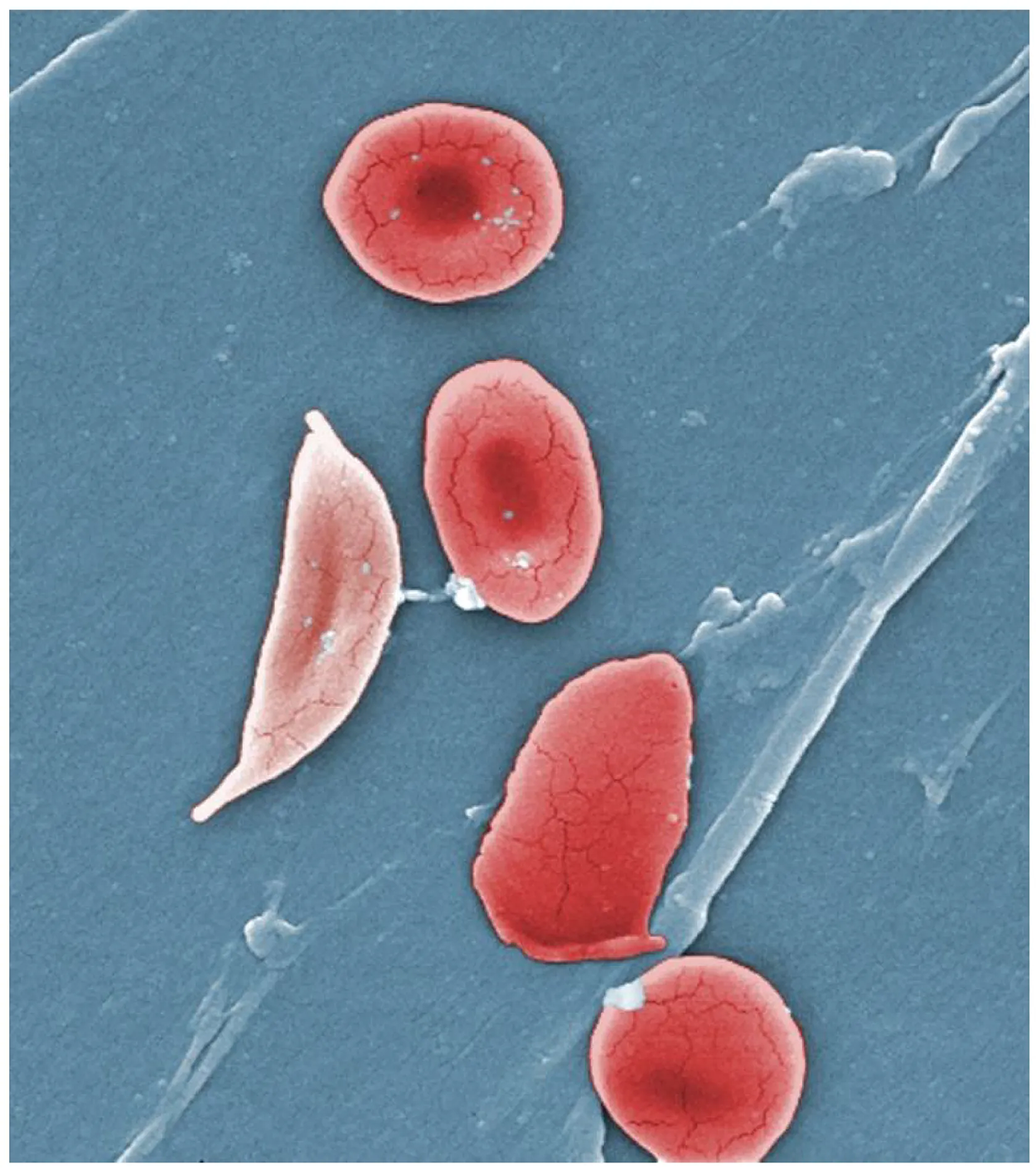
Anemias caused by faulty RBC production or removal include sickle cell anemia, iron deficiency anemia, vitamin deficiency anemia, and diseases of the bone marrow and stem cells.
A mild form of polycythemia is chronic but normal in people living at high altitudes. Some elite athletes train at high elevations specifically to induce this phenomenon. The primary concern with polycythemia is not with oxygen delivery to the tissues, but rather the increased viscosity of the blood, increasing blood pressure and making it more difficult for the heart to circulate the blood.
Thrombocytosis is a condition in which there are too many platelets. This may trigger formation of unwanted blood clots (thrombosis), a potentially fatal disorder. If there is an insufficient number of platelets, called thrombocytopenia, blood may not clot properly, and excessive bleeding may result.
Either an insufficient or an excessive production of platelets can lead to severe disease or death. As discussed earlier, an insufficient number of platelets, called thrombocytopenia, typically results in the inability of blood to form clots. This can lead to excessive bleeding, even from minor wounds.
Another reason for failure of the blood to clot is the inadequate production of functional amounts of one or more clotting factors. This is the case in the genetic disorder hemophilia, which is actually a group of related disorders, the most common of which is hemophilia A, accounting for approximately 80% of cases.
In contrast to the disorders characterized by coagulation failure is thrombocytosis, also mentioned earlier, a condition characterized by excessive numbers of platelets that increases the risk for excessive clot formation, known as thrombosis. A thrombus (plural, thrombi) is an aggregation of platelets, erythrocytes, and even WBCs typically trapped within a mass of fibrin strands.
While the formation of a clot is normal following blood vessel damage, thrombi can form within an intact or only slightly damaged blood vessel. In a large vessel, a thrombus will adhere to the vessel wall and decrease the flow of blood and is referred to as a mural thrombus. In a small vessel, it may completely block the flow of blood and is termed an occlusive thrombus.
Thrombi are most commonly caused by vessel damage to the endothelial lining, which activates the clotting mechanism. These may include venous stasis, when blood in the veins, particularly in the legs, remains stationary for long periods.
Thrombophilia, also called hypercoagulation, is a condition in which there is a tendency to form a thrombus. This may be familial (genetic) or acquired. Acquired forms include the autoimmune disease lupus, immune reactions to heparin, polycythemia vera, thrombocytosis, sickle cell disease, pregnancy, and even obesity. A thrombus can seriously impede blood flow to or from a region and will cause a local increase in blood pressure. If flow is to be maintained, the heart will need to generate greater pressure to overcome the resistance.
When a portion of a thrombus breaks free from the vessel wall and enters the circulation, it is referred to as an embolus. An embolus that is carried through the bloodstream can be large enough to block a vessel critical to a major organ. When it becomes trapped, an embolus is called an embolism. In the heart, brain, or lungs, an embolism may accordingly cause a heart attack, a stroke, or a pulmonary embolism. These are medical emergencies.
Among the many known biochemical activities of aspirin is its role as an anticoagulant. Aspirin (acetylsalicylic acid) is very effective at inhibiting the aggregation of platelets.
EXAMPLE
Aspirin is routinely administered during a heart attack or stroke to reduce the adverse effects. Physicians sometimes recommend that patients at risk for cardiovascular disease take a low dose of aspirin on a daily basis as a preventive measure. However, aspirin can also lead to serious side effects, including increasing the risk of ulcers. A patient should consult a physician before beginning any aspirin regimen.A class of drugs collectively known as thrombolytic agents can help speed up the degradation of an abnormal clot. If a thrombolytic agent is administered to a patient within 3 hours following a thrombotic stroke, the patient’s prognosis significantly improves.
However, some strokes are not caused by thrombi, but by hemorrhage. Thus, the cause must be determined before treatment begins. Tissue plasminogen activator is an enzyme that catalyzes the conversion of plasminogen to plasmin, the primary enzyme that breaks down clots. It is released naturally by endothelial cells but is also used in clinical medicine. New research is progressing using compounds isolated from the venom of some species of snakes, particularly vipers and cobras, which may eventually have therapeutic value as thrombolytic agents.
Leukopenia is a condition in which too few leukocytes are produced. If this condition is pronounced, the individual may be unable to ward off disease. Excessive leukocyte proliferation is known as leukocytosis. Although leukocyte counts are high, the cells themselves are often nonfunctional, leaving the individual at increased risk for disease.
As you learned in a previous lesson, leukemia is a cancer involving an abundance of leukocytes. It may involve only one specific type of leukocyte from either the myeloid line (myeloid leukemia) or the lymphoid line (lymphocytic leukemia). In chronic leukemia, mature leukocytes accumulate and fail to die. In acute leukemia, there is an overproduction of young, immature leukocytes. In both conditions, the cells do not function properly.
Lymphoma is a form of cancer in which masses of malignant (referring to the presence of cancerous cells) T and/or B lymphocytes collect in lymph nodes, the spleen, the liver, and other tissues. As in leukemia, the malignant leukocytes do not function properly, and the patient is vulnerable to infection. Some forms of lymphoma tend to progress slowly and respond well to treatment. Others tend to progress quickly and require aggressive treatment, without which they are rapidly fatal.
Toxemia is the spreading of toxins in the bloodstream and is also sometimes known as blood poisoning. In this disorder, metabolic wastes are not properly removed. Different organs and structures in your body usually take care of metabolic waste and dispose of it properly, but when this does not happen, that metabolic waste will build up in your blood.
This can lead to:
EXAMPLE
A staph infection is a type of bacterial infection caused by the bacteria Staphylococcus aureus. MRSA (methicillin-resistant Staphylococcus aureus) is a type of staph infection that is resistant to many antibiotics and is prevalent in hospitals and other healthcare settings.SOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION. LICENSE: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.