Table of Contents |
Genetics and the environment are factors that can contribute to a congenital disorder, or an abnormality present at birth. Common congenital disorders include heart defects, clubfoot, and cleft palate (CDC, 2024c). Approximately 3% of infants born within the United States have a congenital disorder, and disorders affecting the heart, lungs, or other vital organs account for nearly 20% of infant deaths (CDC, 2024c). Worldwide, congenital disorders affect approximately 3%–6% of all pregnancies (World Birth Defects Day 2023: Global Efforts to Raise Awareness and Support Families | CDC, 2024d). The mortality rate due to congenital disorders worldwide was estimated to be about 7.6% in 2020 (Perin et al., 2023).
Any disease, drug, or other environmental agent that can harm the embryo or the fetus physically or influence health or behavior after birth is called a teratogen. Generally, the influence of a teratogen on a body part is strongest when that part is developing, such as during organogenesis. After organs have formed, they are usually less vulnerable to teratogens, except for the nervous system, which is always susceptible. Limb formation and other aspects of prenatal development show varied critical and sensitive periods for risk of harm from teratogens.
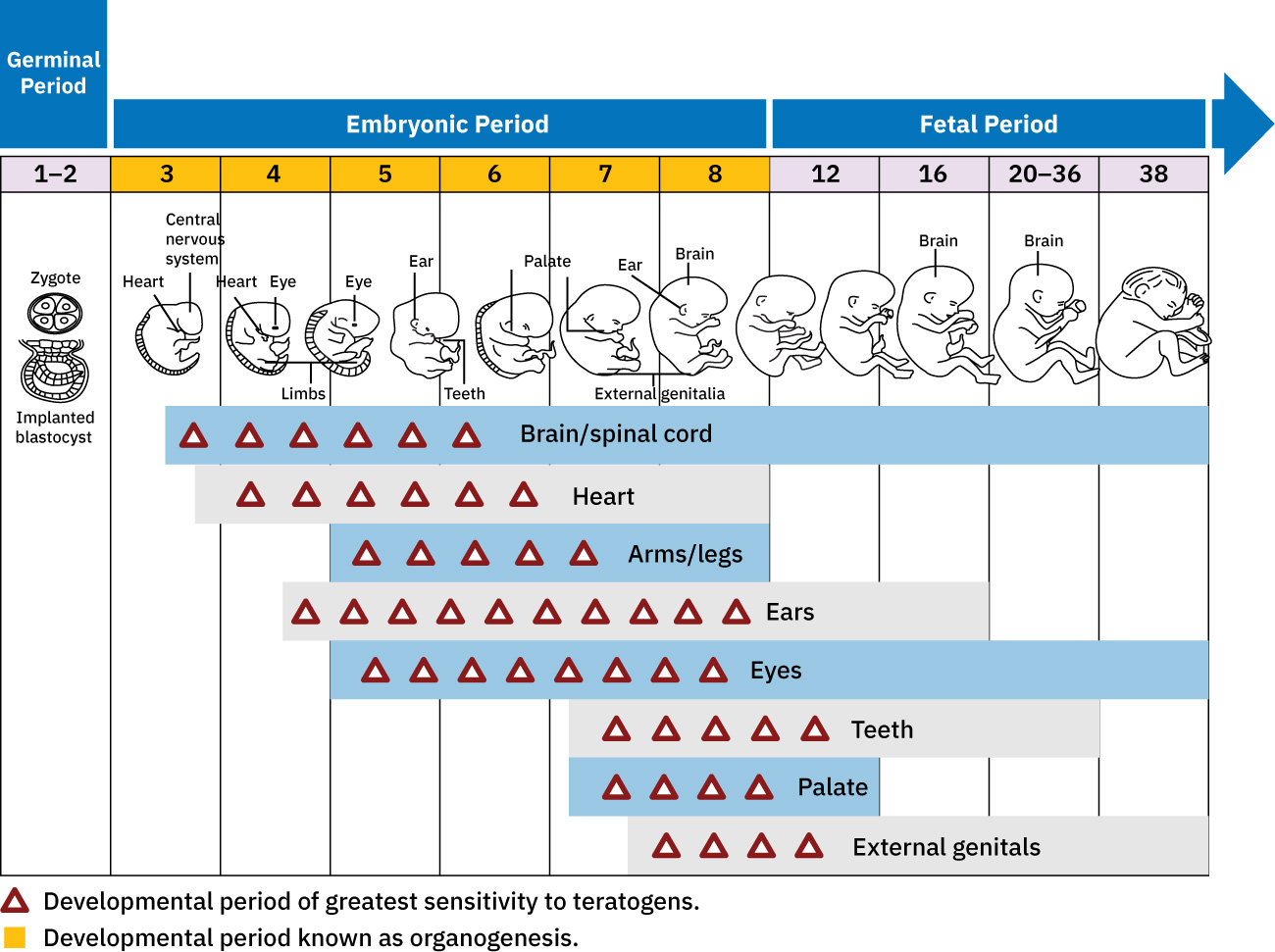
The potential impact of a teratogen varies based on a range of factors including the specific teratogen, the length and amount of exposure, genetic susceptibility, and the quality of the prenatal environment. The longer the exposure or the higher the dose of a teratogen, the greater the likelihood of it doing harm. Some teratogens can cause a range of developmental issues, and in some cases, different teratogens contribute to a specific disorder. Embryos and fetuses can be harmed by teratogens to which their biological fathers were exposed, as well as by those to which they are exposed via the birth mother’s body during gestation.
The long-term effects of some teratogens often depend on the quality of the postnatal environment.
EXAMPLE
Maternal exposure to pollution is related to low birth weight, preterm birth, and neurological effects (Rani & Dhok, 2023). All these put a developing child at increased risk of challenges to overall health and quality of life.| Long-Term Impacts of Various Teratogens | |
|---|---|
| Teratogen | Possible Consequences of Exposure |
| Environmental Toxin | |
| Radiation | Organ anomalies, slowed growth, or nervous system abnormalities depending on exposure timing. |
| Lead | Increased risk for miscarriage, preterm birth, and low birth weight; damage to brain, kidneys, nervous system; learning or behavior problems. |
| Mercury | Brain damage and hearing and vision problems. |
| Polychlorinated biphenyls (PCBs) | Low birth weight and premature birth. |
| Infectious Diseases | |
| Rubella (German measles) | Malformation of organs or miscarriage if exposed during first 3 months of pregnancy. |
| HIV | Transmission of HIV from the biological mother to infant; antiviral treatment during prenatal period drastically reduces transmission to less than 5%. |
| Cytomegalovirus (CMV) | Central nervous system damage and hearing loss. |
| Genital herpes | Blindness or death if exposed to active herpes lesions in the birth canal. |
| Toxoplasmosis and listeria | Miscarriage, preterm birth, and fetal death, depending on exposure timing. |
| Zika virus | Microencephaly, hearing and vision loss, and intellectual disability. |
| COVID-19 | Preterm birth and neurodevelopmental disorders. |
| Syphilis | Premature birth, low birth weight, and fetal death; congenital diseases. |
| Influenza | Spina bifida, cleft palate, and defects in the neural tube. |
| Medications | |
| Aspirin | Miscarriage if high doses are taken early in pregnancy; increased risk of bleeding if low doses are taken. |
| Certain antibiotics (e.g., streptomycin) | Hearing loss and incomplete development of bones and teeth. |
| Thalidomide | Very short or missing arms and legs and other congenital birth defects when taken during early pregnancy. |
| Certain antiseizure medications | Developmental delays during infancy. |
| Certain antipsychotic medications | Increased risk of heart defects. |
| Certain antidepressant medications | Risk is not clear. |
| Psychoactive Drugs | |
| Cocaine | Low birth weight and placental abruption/separation. |
| Opioids and amphetamine | Preterm birth, reduced growth, heart issues, cognitive and behavioral issues. |
| Nicotine | Low birth weight, premature birth, stillbirth. |
| Alcohol | Damage to developing organs; fetal alcohol spectrum disorder. |
| Heroin | Addiction requiring medical care to overcome withdrawal symptoms; damage to the visual system; long-term behavioral consequences. |
| Cannabis | Decreased growth; deficits in attention and long-term executive function; increased impulsivity. |
| Excessive caffeine | Deficiencies in short-term memory, attention, and impulse control; other neurobehavioral and neurological effects. |
Table sources: CDC, 2024a; CDC, 2024b; Cestonaro et al., 2022; Dack et al., 2022; Giuliani et al., 2022; Honein et al., 2017; Kaleelullah & Garugula, 2021; Lin et al., 2023; Lusskin et al., 2018; Mactier & Hamilton, 2020; Manicklal, 2013; March of Dimes, 2021; Nesheim et al., 2012; Orsolini et al., 2017; Ross et al., 2015)
Early formation of the nervous system depends on the formation of the neural tube. Recall that a groove forms along the dorsal surface of the embryo, which becomes deeper until its edges meet and close off to form the tube. Neurulation is a critical step in early brain development, and if this process does not occur properly, a class of disorders called neural tube defects arise.
IN CONTEXT
Folic Acid
Pregnant people are often advised to take folic acid supplements while trying to get pregnant and during early pregnancy. Folic acid is a form of folate. Recall that folate, a B vitamin, is important to the healthy development of the neural tube. Deficiency of maternal folate in the first weeks of pregnancy can result in neural tube defects. The most common neural tube defects are the result of abnormal neural tube closure, which can be caused by environmental and genetic influences.
Many foods, including orange juice and some cereal grains, are fortified with folic acid. The addition of folic acid to specific food products of general consumption has had an immediate impact on the prevalence of neural tube defects. Despite the efficacy of folic acid supplementation, it is still unclear how folic acid directly prevents neural tube defects.
These defects fall into different classes based on type and severity. In the severest forms such as anencephaly, the neural tube does not close at the anterior end and causes missing regions of the skull and brain. Other examples include encephalocele, when the brain protrudes through the skull, and hydrocephalus, which is characterized by an accumulation of cerebrospinal fluid in the brain.
Spina bifida is one of the most well-known examples of a neural tube defect and occurs when the posterior end of the neural tube does not close fully. Spina bifida can range in severity, causing either a complete opening along the vertebrae of the back or a minor separation in the bones of the vertebrae.
There are three classes of this disorder: occulta, meningocele, and myelomeningocele. The first type, spina bifida occulta, is the mildest because the vertebral bones do not fully surround the spinal cord, but the spinal cord itself is not affected. No functional differences may be noticed, which is what the word occulta means; it is hidden spina bifida. The other two types both involve the formation of a cyst—a fluid-filled sac of the connective tissues that cover the spinal cord called the meninges. “Meningocele” means that the meninges protrude through the spinal column, but nerves may not be involved, and few symptoms are present, though complications may arise later in life. “Myelomeningocele” means that the meninges protrude and spinal nerves are involved, and therefore severe neurological symptoms can be present.
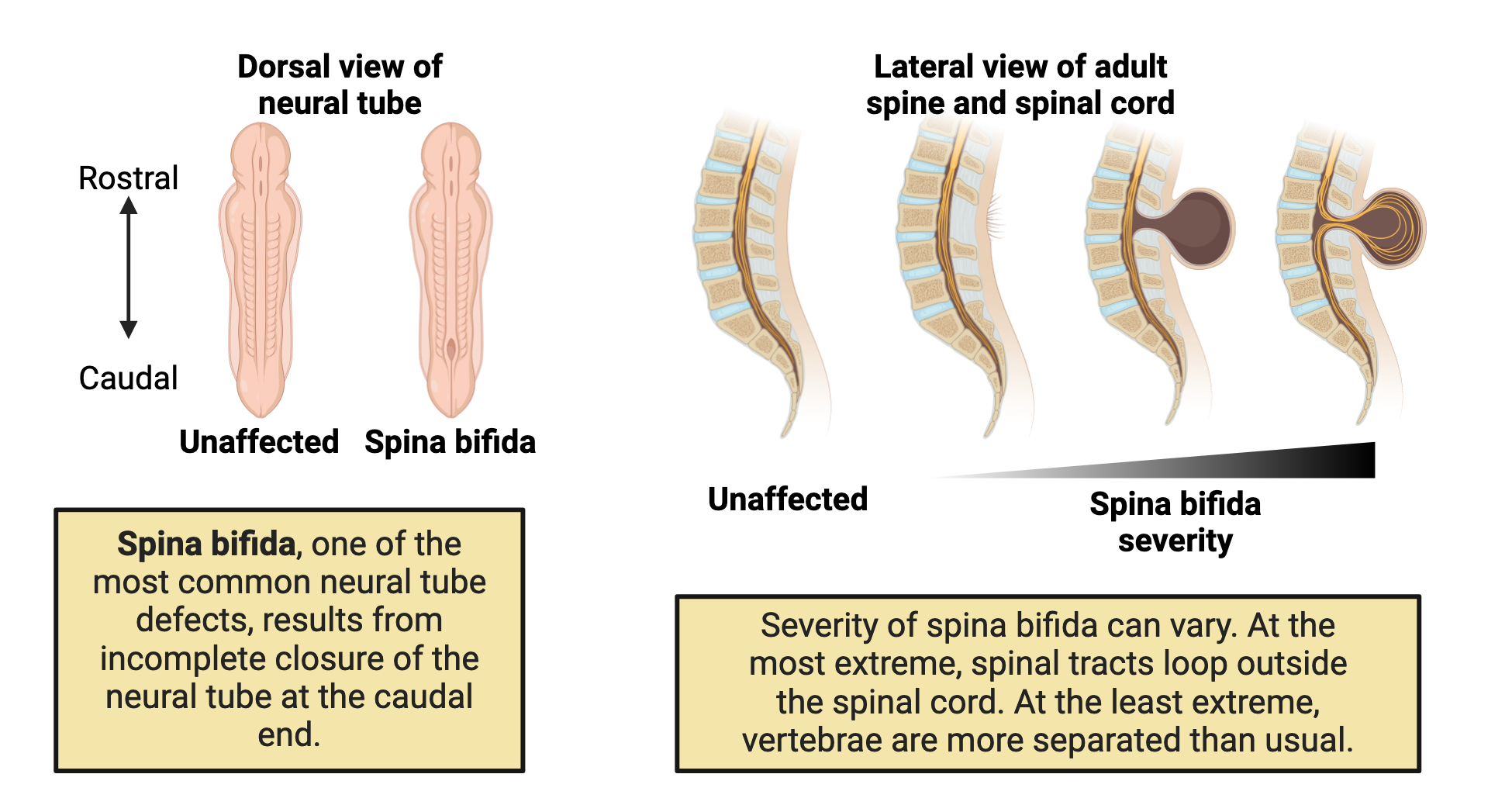
Interestingly, the different types of neural tube defects observed occur at the extreme ends of the neural tube (not in the middle) as a result of how the neural tube closes. The neural tube begins closure in the middle and slowly closes on either end. Spina bifida is localized to the posterior regions of the neural tube, whereas anencephaly, encephalocele, and hydrocephalus occur in the anterior regions of the neural tube.
It is predicted that approximately 70% of neural tube defects occur due to genetic factors. There have been over 240 genes associated with neural tube defects (Harris and Juriloff, 2010), which strongly supports the link between genetic predisposition and neural tube abnormalities. However, genetics do not solely determine the presence of neural tube defects, as a huge proportion of neural tube defects can be prevented with the nutritional supplementation of folic acid in the mother’s diet.
Rubella, toxoplasmosis, and cytomegalovirus (CMV) are examples of disorders that can be caused by infections.
Rubella, or the German measles, is usually a relatively mild viral disease that produces a rash somewhat like that caused by the measles, even though the two diseases are unrelated. Congenital rubella syndrome is the most severe clinical complication of the German measles. This occurs if a person is infected with rubella during pregnancy. The rubella virus is teratogenic, meaning it can cause developmental defects if it crosses the placenta during pregnancy. There is a very high incidence of stillbirth, spontaneous abortion, or congenital birth defects if a person is infected before 11 weeks of pregnancy and 35% if they are infected between weeks 13–16; after this time, the incidence is low. For this reason, prenatal screening for rubella is commonly practiced in the United States. Postnatal infections are usually self-limiting and rarely cause severe complications.
Toxoplasmosis is caused by a parasitic protozoan (Toxoplasma gondii) that causes cysts. Toxoplasma infections in humans are extremely common, but most infected people are asymptomatic or have subclinical symptoms (symptoms that are not distinct or obvious). Toxoplasmosis can also pose a risk during pregnancy because tachyzoites can cross the placenta and cause serious infections in the developing fetus.
The extent of fetal damage resulting from toxoplasmosis depends on the severity of maternal disease, the damage to the placenta, the gestational age of the fetus when infected, and the virulence of the organism. Congenital toxoplasmosis often leads to fetal loss or premature birth and can result in damage to the central nervous system, manifesting as mental retardation, deafness, or blindness. Consequently, pregnant people are advised by the CDC to take particular care in preparing meat, gardening, and caring for pet cats.
IN CONTEXT
If pregnant people have a cat in their house, they're supposed to stay away from the litter box because this parasitic cyst is spread through cat feces.
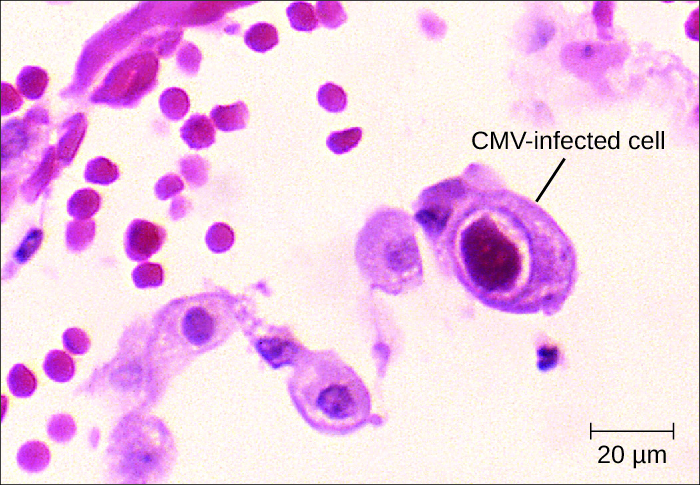
Also known as cytomegalovirus (CMV), human herpesvirus 5 (HHV-5) is a virus with high infection rates in the human population. It is currently estimated that 50% of people in the United States have been infected by the time they reach adulthood. CMV is the major cause of non-Epstein-Barr infectious mononucleosis in the general human population. It is also an important pathogen in immunocompromised hosts, including patients with AIDS, neonates, and transplant recipients. Pregnant people with active infections frequently pass this virus to their fetus, resulting in congenital CMV infections, which occur in approximately one in every 150 infants in the United States. Infants can also be infected during passage through the birth canal or through breast milk and saliva.
Drinking alcohol during pregnancy can increase the baby’s risk for problems such as fetal alcohol spectrum disorders (FASDs) and sudden infant death syndrome (SIDS). FASDs are completely preventable; if a person does not drink alcohol during pregnancy, their child will not have an FASD (CDC, 2022s). Alcohol use can also lead to miscarriage or stillbirth. Different FASD diagnoses are based on particular symptoms.
| Symptoms of FASD Diagnoses | |
|---|---|
| Diagnosis | Symptoms |
| Fetal alcohol syndrome (FAS) | Central nervous system (CNS) problems, minor facial features, growth problems; problems with learning, memory, attention span, communication, vision, and/or hearing. |
| Alcohol-related neurodevelopmental disorder (ARND) | Intellectual disabilities; problems with behavior and learning. May have difficulties in school, particularly with math, memory, attention, judgment, and poor impulse control. |
| Alcohol-related birth defects (ARBD) | May have problems with the heart, kidneys, bones, and/or hearing. |
| Neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE) |
The pregnant person must have consumed more than 13 alcoholic drinks per month of pregnancy (that is, any 30-day period of pregnancy) or more than two alcoholic drinks in one setting. For diagnosis with ND-PAE, the child must have problems in:
|
Smoking can have adverse health effects before, during, and after pregnancy. The CDC (2020a) indicates that people who smoke tobacco have more difficulty becoming pregnant. Smoking tobacco during pregnancy can lead to preterm birth, low birth weight, miscarriage, congenital disorders, and SIDS. Pregnant people exposed to secondhand smoke are more likely to have low birth weight babies. Babies exposed to secondhand tobacco smoke are more likely to die from SIDS and have weaker lungs, which can lead to additional health problems (CDC, 2020a). Pregnant people who smoke marijuana may double their risk of stillbirth; using marijuana during pregnancy can interfere with fetal brain development (Chang, 2023).
People who use other drugs during pregnancy can experience problems with fetal and infant health. Use of opioids such as heroin, diverted or misused prescription opioids, or other morphine-like drugs is associated with substantial maternal, fetal, and neonatal risks (Seligman et al., 2023). Cocaine use by the pregnant client also leads to preterm birth and LBW. Methamphetamine exposure during pregnancy has been associated with maternal and neonatal morbidity and mortality (Chang, 2023). Self-reported data from 2019 indicated that 6.6% of pregnant clients reported prescription opioid use during pregnancy, and 21.2% of these reported drug misuse (Ko et al., 2020). The drug overdose mortality rate per 100,000 for pregnant or postpartum persons almost doubled from 2017 (6.56) to 2020 (11.85) in the United States (Bruzelius & Martins, 2022).
Neonatal abstinence syndrome (NAS) is a treatable condition in newborns exposed to certain drugs, particularly opioids, while in utero. The term neonatal opioid withdrawal syndrome (NOWS) specifically describes the symptoms experienced by infants exposed to opioids. Both NAS and NOWS include intense irritability, difficulty with feeding, respiratory issues, and seizures.
Physicians use a variety of methods to monitor the development and health of the growing fetus. You will learn about a few of these approaches here. Not only do these allow us to observe the development of structures and organs, but some can detect the presence of chromosomal abnormalities:
SOURCE: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “ANATOMY AND PHYSIOLOGY 2E”. ACCESS FOR FREE AT OPENSTAX.ORG/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E/PAGES/1-INTRODUCTION. LICENSE: CREATIVE COMMONS ATTRIBUTION 4.0 INTERNATIONAL.