Table of Contents |
Hair is an accessory structure of the integumentary system that functions to protect the body from cold and harmful organisms. It is primarily made of dead, keratinized cells that are generated from tissue of the epidermis. Hair is grown in and extends out of a specialized cavity in the skin called a hair follicle. The majority of hair follicle is located in the dermis of the skin. However, as you can see in the image below, it is formed by epidermal tissue that has extended deep into the dermis. As hair grows, it extends out of the skin and into the surrounding external environment.
The hair shaft is the part of the hair not attached to the surrounding tissue of the follicle. Much of the hair shaft is exposed outside of the skin surface. This is the hair that you see on your arm or head. The rest of the hair, which is attached to the tissue of the follicle, lies below the surface of the skin and is referred to as the hair root. The hair root ends deep in the dermis at the expansion of the hair follicle called the hair bulb. Inside of the hair bulb are basal cells, collectively called the hair matrix, which function like the basal cells of the stratum basale, actively dividing to produce new keratinocytes. The hair bulb surrounds the hair papilla, which is made of connective tissue and contains blood capillaries and nerve endings from the dermis, supplying nutrients, waste removal, and communication to the hair matrix.
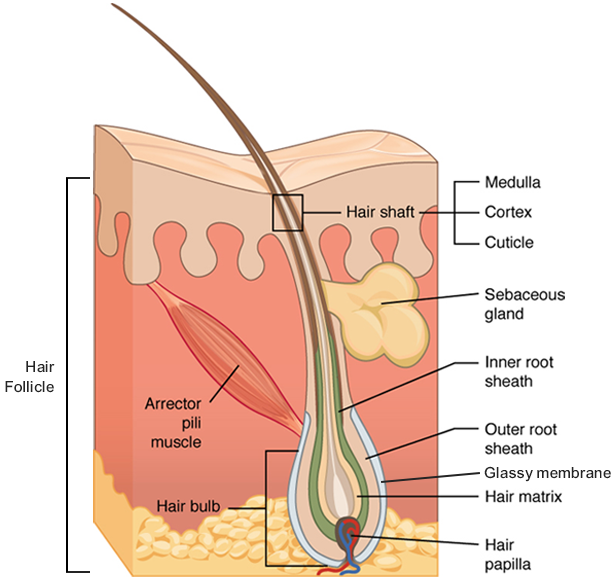
Just as the basal layer of the epidermis forms the layers of epidermis that get pushed to the surface as the dead skin on the surface sheds, the basal cells of the hair bulb divide and push cells outward in the hair root and shaft as the hair grows. Each hair is composed of three layers of keratinocytes. The medulla forms the innermost layer of the hair, which is surrounded by the cortex, a layer of compressed, keratinized cells that is covered by an outer layer of very hard, keratinized cells known as the cuticle.
The wall of the hair follicle is made of three concentric layers of cells. The cells of the internal root sheath surround the root of the growing hair and extend just up to the hair shaft. They are derived from the basal cells of the hair matrix. The external root sheath, which is an extension of the epidermis, encloses the hair root. It is made of basal cells at the base of the hair root and tends to be more keratinous in the upper regions. The glassy membrane is a thick, clear connective tissue sheath covering the hair root, connecting it to the tissue of the dermis.
Hair serves a variety of functions, including protection, sensory input, thermoregulation, and communication. For example, hair on the head protects the skull from the sun.
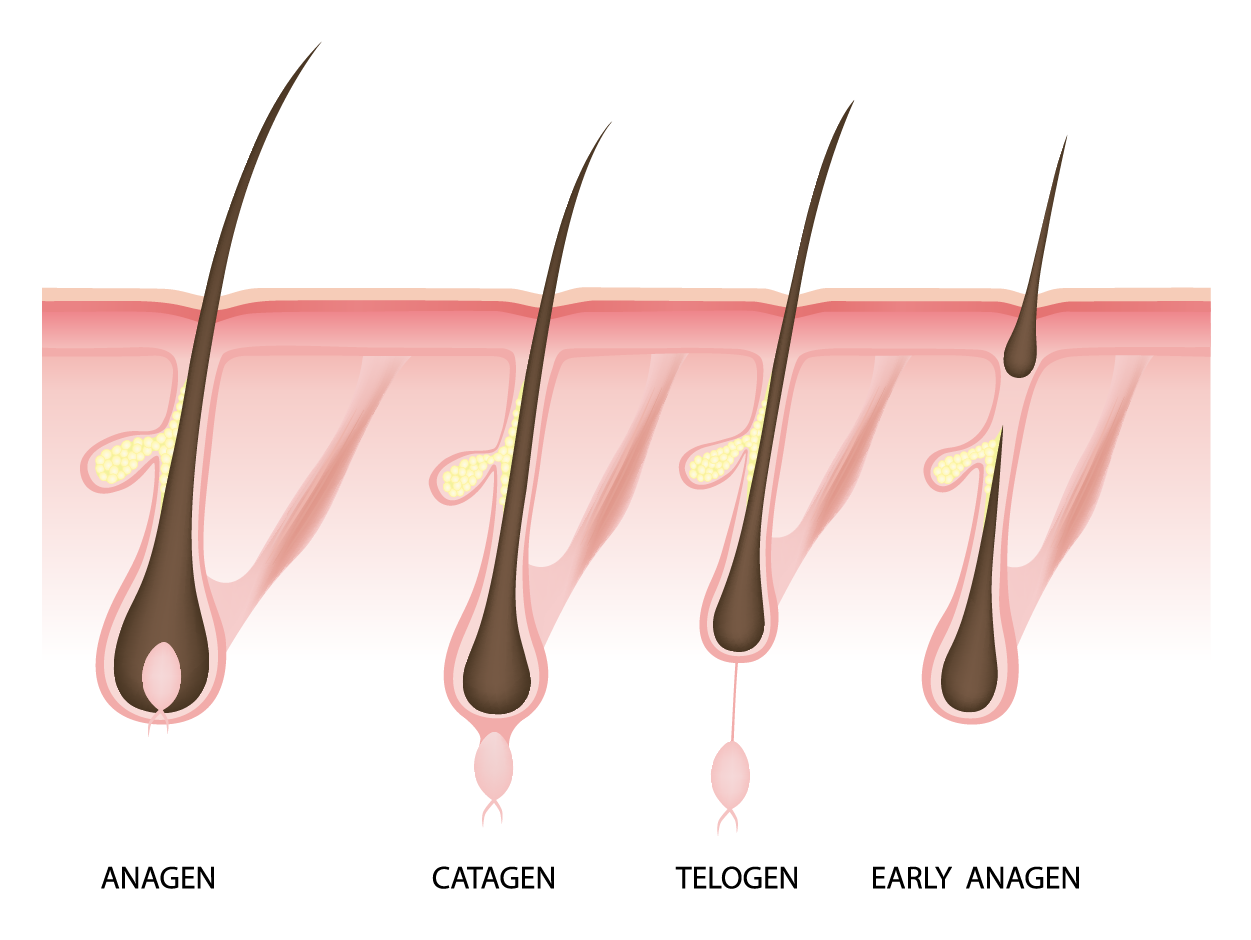
Hair grows and is shed in a cyclic pattern. This occurs in three phases. The first is the anagen phase, during which cells divide rapidly at the root of the hair, pushing the hair shaft up and out. The length of this phase is measured in years, typically from 2 to 7 years. The catagen phase lasts only 2 to 3 weeks, and marks a transition from the hair follicle’s active growth. During this phase, the existing hair disconnects from the hair matrix and becomes a club hair. Finally, during the telogen phase, the hair follicle is at rest and no new growth occurs. At the end of this phase, which lasts about 2 to 4 months, another anagen phase begins. The basal cells in the hair matrix then produce a new hair follicle, which pushes the club hair out as the growth cycle repeats itself. Hair typically grows at the rate of 0.3 mm per day during the anagen phase. On average, 50 hairs are lost and replaced per day. Hair loss occurs if there is more hair shed than what is replaced and can happen due to hormonal or dietary changes. Hair loss can also result from the aging process or the influence of hormones.

Similar to the skin, hair gets its color from the pigment melanin, produced by melanocytes in the hair papilla. Different hair color results from differences in the type of melanin, which is genetically determined. Recall that melanin can produce colors ranging from red to yellow to brown to black.
As a person ages, melanin production decreases, and hair tends to lose its color and becomes gray and/or white. Melanin production can also be changed under periods of stress.
Nails are an accessory structure of the integumentary system which functions to protect the body from damage at the tips of the fingers and toes. The nail is formed by highly keratinized, dead stratified squamous epithelial tissue generated by an active stratum basale at the nail root deep within the proximal edge of the nail. As new cells are produced, the nail is pushed forward, creating growth. The large central portion of the nail is called the nail body (or nail plate) and protects the underlying tissue at the distal end of the finger. The epithelial tissue that the nail body lays on top of is called the nail bed. As the nail extends beyond the distal edge of the finger, it forms the free edge. This is the part of the nail that you cut with nail clippers.
The nail itself is embedded into the skin of the finger. The lateral edges of the nail are covered by the lateral nail folds while the proximal edge of the nail coming from the nail root is covered by the proximal nail fold. The proximal nail fold produces a clear layer of skin called the eponychium, commonly called the cuticle. Underneath the free edge, the skin creates another clear layer of skin called the hyponychium. These structures keep dirt, bacteria, or other substances from finding their way underneath the skin at the fingertips.
The nail bed is rich in blood vessels, making it appear pink, except at the base, where a thick layer of epithelium over the nail matrix forms a crescent-shaped region called the lunula (the “little moon”).
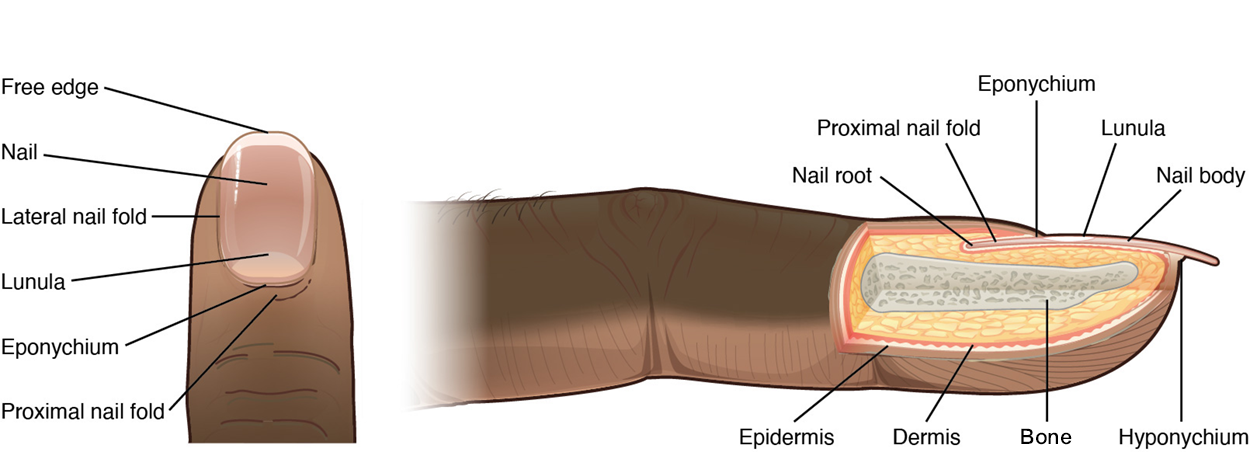
Nails function to reinforce the distal end of the fingers and toes and protect them from pressure. If a nail is lost due to damage, it will grow back so long as the nail root is intact. As a new nail grows, it is possible that the lateral edge of the nail may grow further into the lateral nail fold than it should. This is called an ingrown nail. If caught early, the nail edge can be physically removed from the nail edge. If allowed to grow, this can lead to infections and pain.
Recall that exocrine glands are epithelial structures that produce and release secretions that have a direct pathway to the outside of the body. The integumentary system has two accessory structures that are exocrine glands—sweat glands and oil glands.
When the body becomes warm, the skin has a gland called the sudoriferous gland, also known as sweat gland, that can help to cool the body. Sweat glands develop from epidermal projections into the dermis and are classified as merocrine glands; that is, the secretions are excreted by exocytosis through a duct without affecting the cells of the gland. There are two types of sweat glands, each secreting slightly different products.
An eccrine sweat gland is a type of sudoriferous gland that produces a hypotonic sweat primarily meant to regulate body temperature, a process called thermoregulation. These glands are active from birth and are found all over the skin’s surface but are especially abundant on the palms of the hand, the soles of the feet, and the forehead. They are coiled glands lying deep in the dermis, with the duct rising up to a pore on the skin surface, where the sweat is released. This type of sweat is composed mostly of water, with some salt, antibodies, traces of metabolic waste, and an antimicrobial peptide. Eccrine glands are a primary component of thermoregulation in humans and thus help to maintain homeostasis. However, they also serve to wash the skin and limit the growth of harmful bacteria on the skin's surface.
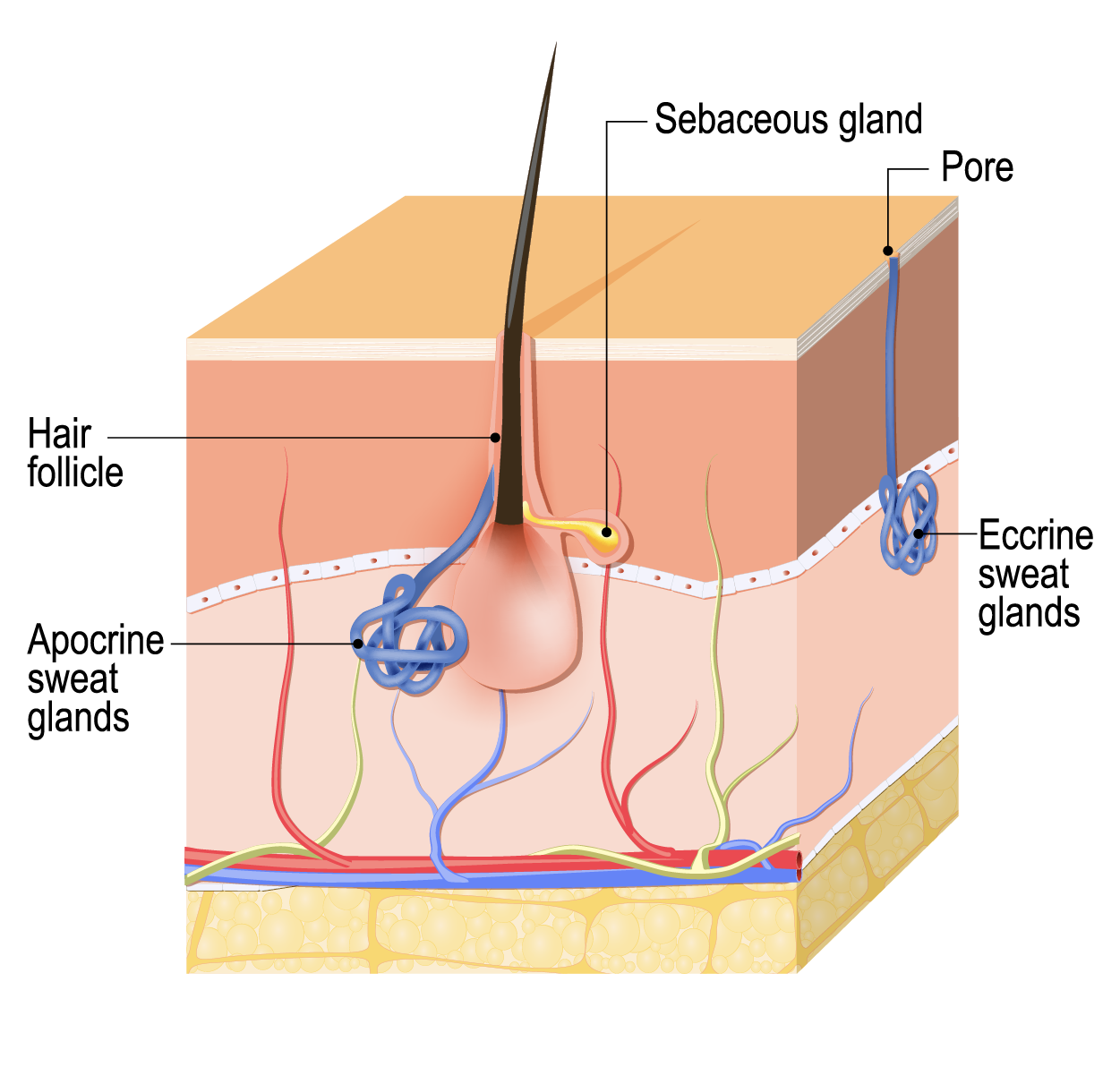
An apocrine sweat gland is a sudoriferous gland typically associated with hair follicles in densely hairy areas, such as armpits and genital regions. Apocrine sweat glands are larger than eccrine sweat glands and lie deeper in the dermis, sometimes even reaching the hypodermis, with the duct normally emptying into the hair follicle. These glands are also not active until puberty. In addition to water and salts, apocrine sweat includes organic compounds that make the sweat thicker and provide bacteria on the skin surface with metabolic nutrients (proteins, lipids). The smell associated with these sweat glands comes not from the secreted sweat but from the byproducts of bacterial metabolism. However, despite its negative social connotation (who likes to smell like an armpit?), the release of this sweat is under both nervous and hormonal control and plays a role in the poorly understood human pheromone response. Pheromones are chemicals secreted to influence the behavior of others such as attracting a mate, warning an enemy, etc.
A sebaceous gland is a type of oil gland that is found all over the body and helps to lubricate and waterproof the skin and hair. Most sebaceous glands are associated with hair follicles. They generate and excrete sebum, a mixture of lipids, onto the skin surface, thereby naturally lubricating the dry and dead layer of keratinized cells of the stratum corneum, keeping it pliable. The fatty acids of sebum also have antibacterial properties and prevent water loss from the skin in low-humidity environments. The secretion of sebum is stimulated by hormones, many of which do not become active until puberty. Thus, sebaceous glands are relatively inactive during childhood.
Source: THIS TUTORIAL HAS BEEN ADAPTED FROM OPENSTAX “ANATOMY AND PHYSIOLOGY 2E.” ACCESS FOR FREE AT HTTPS://OPENSTAX.ORG/DETAILS/BOOKS/ANATOMY-AND-PHYSIOLOGY-2E. LICENSE: CC ATTRIBUTION 4.0 INTERNATIONAL.